Dysautonomia and POTS: If you’re living with dysautonomia or Postural Orthostatic Tachycardia Syndrome (POTS), you know how quickly a “normal” day can turn into a marathon of dizziness, racing heart, brain fog, and sheer exhaustion. You might feel unheard, shuffled between specialists, or told “everything looks fine” when your body says otherwise.
At Lavender Family Chiropractic in Sarasota, our three-doctor upper cervical team—Dr. Rusty Lavender, Dr. Jacob Temple, and Dr. Will Guzinski—meets people like you every week. Many have tried “everything,” yet still struggle. Our approach is different: gentle, precise, and focused on the top of the neck (the atlas), where the brainstem and vagus nerve live—gatekeepers for the autonomic nervous system that regulates heart rate, blood pressure, digestion, temperature control, and more.
This in-depth guide explains dysautonomia and POTS in clear terms, why atlas misalignment may contribute to autonomic dysfunction, and how upper cervical chiropractic care aims to restore healthy signaling—so your body can do what it’s designed to do. You’ll also find practical self-care tips, real-world expectations, and a comprehensive FAQ. If you’re searching for a “chiropractor Sarasota Florida,” “upper cervical chiropractor near me,” “Vertigo doctor near me,” or even “Migraine doctor near me,” you’re in the right place.
What Are Dysautonomia and POTS?
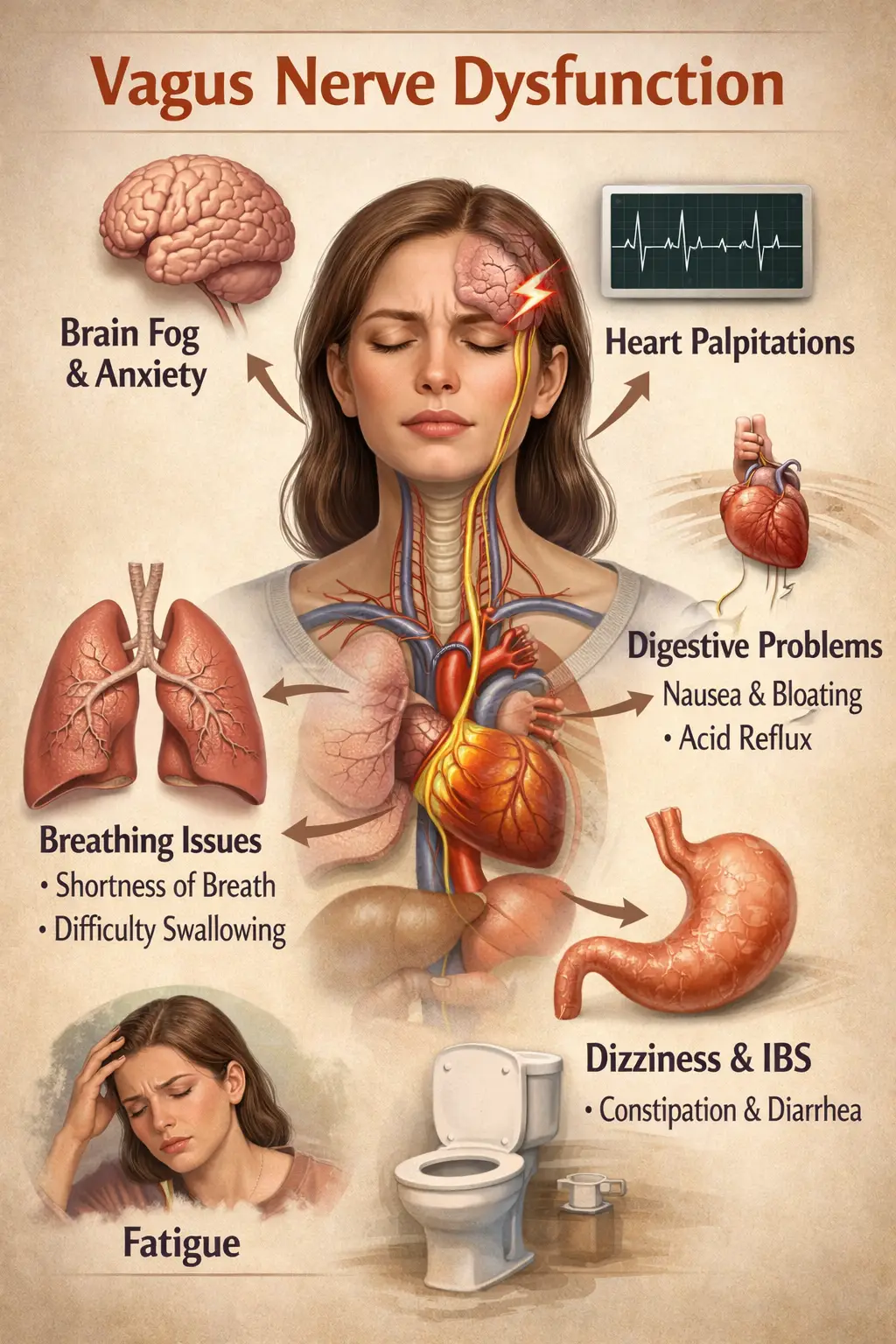
Dysautonomia is an umbrella term for conditions involving dysfunction of the autonomic nervous system (ANS). The ANS regulates automatic processes like blood pressure, heart rate, breathing patterns, digestion, and pupillary responses—essentially, your body’s autopilot. When the ANS misfires, you may experience fluctuating blood pressure, rapid heartbeat, fainting or near-fainting, GI distress, temperature intolerance, and more.
POTS (Postural Orthostatic Tachycardia Syndrome) is one of the most recognized forms of dysautonomia. It’s characterized by an excessive heart rate increase—often 30+ beats per minute in adults—within 10 minutes of standing, usually accompanied by symptoms like dizziness, lightheadedness, palpitations, and fatigue. Many patients also describe “adrenaline surges,” anxiety-like sensations, and cognitive “brain fog.”
POTS can be triggered or worsened by illness, injury (including concussions and whiplash), significant stress, hormonal shifts, or periods of deconditioning. Importantly, POTS is not “just in your head.” It’s a physiology problem—often multifactorial—requiring a compassionate, systems-based plan.
Common Symptoms of POTS and Dysautonomia
Not everyone has the same pattern, but these are frequently reported:
- Orthostatic intolerance (worse when standing): dizziness, lightheadedness, near-syncope, or fainting.
- Rapid heart rate with minimal exertion or upon standing (palpitations, pounding heartbeat).
- “Drop attacks”: sudden collapses or losses of postural control. Some people remain conscious; others feel a quick power-down. It’s frightening, and it deserves attention.
- Headaches and migraines (including vestibular migraines).
- Vertigo, dizziness, and balance problems—commonly described as rocking, swaying, or “boat” sensations.
- Brain fog and poor concentration—difficulty with word-finding, memory, processing speed.
- Fatigue and exercise intolerance—a “battery” that drains fast or crashes after activity.
- GI issues—nausea, bloating, constipation/diarrhea cycles, early fullness (suggesting vagal involvement).
- Temperature dysregulation—heat intolerance, chills, or night sweats.
- Shortness of breath or air hunger.
- Sleep disturbances—trouble falling/staying asleep; non-restorative sleep.
- Visual changes—blurriness, light sensitivity, visual snow.
- Anxiety-like symptoms—often secondary to autonomic surges; many patients report they are not “mentally anxious,” but their body feels revved up.
- Neck pain and stiffness—sometimes following whiplash or trauma.
- Chest pain or tightness, tremulousness, and tingling.
If you recognize several items on this list, especially the orthostatic pattern, your symptoms are valid—and there are steps you can take.
The Atlas, Vagus Nerve, and Brainstem: Why the Top of the Neck Matters
The atlas (C1) is the top vertebra of your spine. It cradles the skull and surrounds the lower brainstem. The vagus nerve (cranial nerve X) exits the brainstem, travels through the jugular foramen, and passes near the upper cervical region on its way to the heart, lungs, and digestive system. The cervical sympathetic chain also runs along the side of the neck, helping regulate vascular tone (how your blood vessels constrict/relax) and heart responses.
Here’s why this matters:
- Brainstem proximity: The area around C1–C2 houses neural centers integral to heart rate, blood pressure, breathing reflexes, and vestibular integration. Subtle biomechanical stress here may influence autonomic tone.
- Vagus nerve pathway: Mechanical irritation or altered tissue tension near the jugular foramen or upper cervical soft tissues can, in theory, perturb vagal signaling—potentially contributing to GI dysmotility, heart-rate variability changes, and “fight-or-flight” bias.
- Baroreflex and proprioception: The atlas region is loaded with proprioceptors—tiny sensors that inform the brain about position and movement. Faulty neck input can disrupt balance, eye stabilization, and cardiovascular reflexes (baroreflex), surfacing as dizziness, visual instability, and orthostatic symptoms.
- Vertebral arteries and CSF dynamics: The vertebral arteries pass through the cervical spine to the brain. While most people compensate just fine, an inefficient upper-cervical alignment can contribute to strain and altered fluid dynamics, which some patients experience as headaches, pressure, or disequilibrium.
- Postural control: Your head is heavy. Even a few millimeters of atlas misalignment can shift global posture, increasing muscular load and sympathetic drive as your body constantly “corrects” its balance. That background stress can amplify dysautonomia symptoms.
Upper cervical chiropractic care focuses precisely here, aiming to restore efficient alignment and reduce aberrant stress at the neurological “neck hub.”
How Atlas Misalignment Can Contribute to POTS-Like Patterns
To be clear, POTS is multifactorial. Not everyone with POTS has an atlas problem—and not everyone with an atlas problem has POTS. But for a meaningful subset, we observe:
- Heightened sympathetic tone (“gas pedal stuck on”): Suboptimal alignment can provoke persistent low-grade irritation around the brainstem and cervical sympathetic pathways. Patients describe feeling revved up, jumpy, or intolerant of heat/exertion.
- Vagus nerve dysregulation (weakened “brake” pedal): If vagal signaling underperforms, heart rate can run high, digestion can slow or spasm, and recovery can lag. Rest-and-digest gives way to go-go-go.
- Proprioceptive mismatch: Faulty neck input to the brain’s balance and cardiovascular centers can create dizziness, visual-vestibular conflict (rocking/swaying), and orthostatic intolerance.
- Muscular and dural tension: Chronic guarding in suboccipital muscles and upper cervical fascia may tug on surrounding structures, reinforcing the cycle.
By restoring a more neutral atlas position, we seek to reduce these inputs, allowing the nervous system to self-regulate more effectively. Many patients report improved steadiness, clearer thinking, calmer heart rate responses, and better tolerance for daily movement.
Upper Cervical Chiropractic 101 (Gentle, Precise, No Popping, Twisting, or Cracking)
Upper cervical chiropractic is a subspecialty focused on the top of the neck—particularly C1 (atlas) and C2 (axis). Unlike general spinal manipulation, upper cervical adjustments are:
- Measured and customized: We analyze your unique bone structure and alignment vectors before any adjustment.
- Low-force and specific: Corrections are gentle and targeted—no twisting or forceful cracking.
- Neuro-focused: We care about how your nervous system is functioning (not just how joints move).
At Lavender Family Chiropractic, we use:
- 3D CBCT imaging (cone beam computed tomography) to see the exact 3D orientation of your atlas/axis and related structures. This is the “blueprint” for precision.
- Functional nervous system scans with Tytron paraspinal infrared thermography to evaluate autonomic patterns along the spine. These scans help us determine whether your system is in balance—or not—and how it responds to care over time.
- Doctor-delivered, gentle corrections—tailored to your measurements. Our goal is to restore alignment and stability, not to “over-adjust.”
Our Process for People with Dysautonomia and POTS
1) Complimentary Consultation
We start with a conversation. We listen to your story—onset, triggers, flares, what helps, what doesn’t. If your case is a good fit for upper cervical care, we move forward.
2) History and Neuro-Ortho Exam
We assess balance, posture, range of motion, neurological reflexes, and autonomic clues (such as skin temperature asymmetries, breath rate patterns, etc.).
3) Tytron Thermography
We perform scan-based analysis to detect autonomic patterning. Over time, these scans help us track whether your system is trending toward regulation.
4) 3D CBCT Imaging
We acquire high-resolution images to quantify your atlas/axis alignment in three dimensions. Every person’s anatomy is different. The math of your misalignment guides the math of your correction.
5) Customized Upper Cervical Adjustment
Your first correction is delivered with precision—no twisting or cracking. Many patients are surprised how gentle it feels.
6) Rest and Re-Check
We allow your system to settle, then reassess to confirm your nervous system responded as expected. You’ll receive a personalized care plan focused on holding your alignment (the longer you hold, the more your body can heal).
7) Re-Evaluations and Outcome Tracking
We re-scan and re-check at intervals. Many patients track heart rate, HRV, step counts, and symptom journals—the objective and subjective views together paint a clearer picture.
What Improvements Do Patients Often Report?
Every person is unique, and results vary. That said, many upper cervical patients with dysautonomia and POTS share the following themes as care progresses:
- Dizziness decreases and episodes are shorter or less intense.
- Brain fog lifts; clarity and word-finding improve.
- Better heart-rate responses to standing, walking, and light exercise.
- Fewer migraines/headaches or reduced severity.
- Improved sleep quality and more consistent energy.
- Less GI turbulence (nausea, bloating, “nervous stomach” calm down).
- Greater tolerance to heat or busy environments.
- Increased confidence with daily tasks and social activities.
We never promise a cure. We focus on restoring alignment and regulation so your body can do more of the healing work it’s designed to do.
The Role of Collaboration: Medical Care + Upper Cervical Care
Upper cervical care pairs well with medical management. Many POTS patients work with cardiologists, neurologists, primary care physicians, and physical therapists. We encourage a team approach. You may continue medications while exploring conservative, non-invasive care; your prescribing physician manages those decisions. We can also share progress notes to promote coordinated care.
Practical Self-Care Tips for POTS and Dysautonomia
These general strategies are widely discussed among patients and providers. Always personalize with your healthcare team:
- Hydration & salt (if appropriate): Electrolyte-rich fluids can support blood volume. Confirm amounts with your provider.
- Compression garments: Waist-high compression can reduce blood pooling in the legs.
- Paced breathing / vagal toning: Slow exhalations, “box breathing,” and gentle humming can encourage parasympathetic activity.
- Recumbent exercise and gradual conditioning: Start with rowing or a recumbent bike, then progress as tolerated.
- Frequent small meals: Large meals can worsen post-meal fatigue and tachycardia; lighter meals may help.
- Sleep routine: Consistent bed and wake times, dark/cool room, and wind-down rituals.
- Heat strategies: Cooling towels, portable fans, and shaded breaks.
- Postural pacing: Rise slowly from sitting/lying; avoid standing still for long periods.
- Neck care: Mind your ergonomics and pillow fit; ask us about Pillowwise-style sizing options if appropriate.
These do not replace care, but they set the stage for your nervous system to respond better.
Why Choose Lavender Family Chiropractic (Sarasota • Lakewood Ranch • Bradenton)
- Upper Cervical Specialists: Our entire practice is built around atlas-focused care.
- Three-Doctor Team: Dr. Rusty Lavender, Dr. Jacob Temple, and Dr. Will Guzinski collaborate on complex cases.
- 3D CBCT + Tytron Scans: Precision imaging and functional nervous system scans guide every step.
- Gentle, Precise Adjustments: No popping, twisting, or cracking—ever.
- Comfort and Follow-Through: From zero-gravity rest chairs to measured re-checks, we obsess over details that support healing.
- Local + Accessible: If you’re searching for a “chiropractor near me,” “upper cervical chiropractor near me,” “Vertigo doctor near me,” or “Migraine doctor near me,” our Sarasota location serves the greater region with convenient access.
Address: 5899 Whitfield Ave Ste 107, Sarasota, FL 34243
Phone: (941)243-3729
Website: www.chiropractorsarasotaflorida.com
Service Areas: Sarasota, Bradenton, Lakewood Ranch, Parrish, Ellenton, Venice, Osprey, Punta Gorda, St. Petersburg, Siesta Key, Longboat Key, Lido Key, and Myakka City.
Case Snapshots (Anonymized, Illustrative)
Case A: The College Athlete
After a viral illness, a student developed classic POTS patterns: HR jumps 40+ bpm on standing, dizziness, brain fog, and daily headaches. CBCT showed a right-sided atlas rotation with inferior tilt; Tytron scans revealed persistent autonomic patterning. After precise upper cervical care and a graded recumbent exercise plan, she reported steadier mornings, fewer headaches, and a calmer heart rate with standing. By month three, she tolerated light interval training without crashes.
Case B: The Busy Parent
Following a car accident, a parent developed neck pain, vertigo spells, “drop attacks,” and an anxiety-like internal buzz. Atlas misalignment was significant on imaging. After gentle corrections and postural pacing strategies, vertigo decreased, drop attacks ceased, and sleep improved. He now completes school pickups and errands without fear of sudden collapse.
Case C: The Remote Professional
Years of desk work plus a concussion in the past led to worsening orthostatic symptoms and constant brain fog. With alignment restored and an ergonomics reset, fog lifted, headaches eased, and productivity returned. She still manages hydration, salt, and compression—but now enjoys longer “good windows” each day.
These stories are not guarantees. They reflect what we commonly observe when alignment is part of the picture.
How Upper Cervical Care Supports the Vagus Nerve
Think of the vagus nerve as the brake pedal for your autonomic system. When atlas alignment is efficient and tissues are calm, the environment around the brainstem and vagus pathway is less irritated. Many patients notice:
- Better digestion rhythms and less nausea.
- Calmer heart rate between tasks (improved heart-rate variability patterns).
- Easier downshifting at night for sleep.
In other words, we don’t treat POTS—we restore mechanical and neurological efficiency at a critical control center so your body can self-regulate more effectively.
Who Is (and Isn’t) a Good Candidate?
You’re likely a good candidate if you:
- Have dysautonomia/POTS symptoms plus a history of neck strain, whiplash, concussion, or persistent neck stiffness.
- Notice that head/neck position or long desk days flare your symptoms.
- Want a conservative, non-pharmaceutical approach to complement your medical care.
You may not be a candidate if you have red flags that require immediate medical attention or if imaging/exam suggests your symptoms do not relate to upper cervical mechanics. In those cases, we’ll guide you to appropriate providers.
What to Expect in the First Month
- Week 1–2: Foundational corrections, rest, and initial pattern changes. Some patients feel lighter or calmer right away; others need time as tissues adapt.
- Week 3–4: We aim for stability—holding the correction is the goal. Re-scans help us decide if/when to adjust again. You’ll likely implement home strategies (hydration, breathing, recumbent cardio).
- By 4–6 weeks: Many report improved steadiness, fewer acute spikes, and more “green-light” periods. For chronic or complex cases, progress often continues over months as the nervous system re-trains.
Top 15 FAQs About Dysautonomia, POTS, and Upper Cervical Care
1) Is upper cervical chiropractic a cure for POTS?
No. We don’t claim to cure POTS. We correct atlas misalignments that may contribute to autonomic dysregulation. Many patients experience meaningful improvements, but results vary.
2) How do you know if my atlas is misaligned?
We use 3D CBCT imaging to measure your unique alignment and Tytron thermography to assess autonomic patterns. Together, these guide precise corrections and progress checks.
3) Will you “crack” my neck?
No. Our corrections are gentle and specific—no popping, twisting, or cracking.
4) Can upper cervical care help “drop attacks”?
When drop attacks are related to cervical/vestibular triggers or brainstem stress, some patients report fewer episodes as alignment stabilizes. We evaluate your history to determine fit and collaborate with your medical team.
5) How soon will I notice changes?
Some feel shifts in the first 1–3 visits (steadier head, calmer system). Others need several weeks. Chronic cases may improve gradually over months. Our focus is on holding alignment—healing often follows stability.
6) Will I need adjustments forever?
No. Our goal is fewer adjustments that last longer. Once you’re stable, we transition to maintenance check-ins to keep you steady through life’s curveballs.
7) Can I continue my medications?
Yes. Medication decisions are managed by your prescribing physician. We coordinate care and share updates as needed.
8) Is this safe if I’m hypermobile (e.g., hEDS)?
We tailor care for tissue sensitivity and ligament laxity. Gentle, specific corrections are often well-tolerated. We’ll review your case in detail.
9) What if I’ve had prior neck surgery or serious injury?
We evaluate surgical history and imaging carefully. Some postsurgical cases are appropriate for upper cervical care; others are not. If we’re not the right fit, we’ll refer you.
10) Do you help with migraines, vertigo, and TMJ too?
Yes. Many patients come for migraines, vestibular disorders, TMJ, and neck pain—conditions often intertwined with upper cervical mechanics and autonomic regulation.
11) How does this differ from general chiropractic?
Upper cervical is a precision subspecialty focused on C1/C2 with detailed imaging, vector analysis, and gentle corrections—no twisting/cracking of the full spine.
12) Will I have to change my lifestyle?
We’ll suggest nervous-system-friendly habits (hydration, breathing, pacing, recumbent exercise). Most are simple, sustainable, and tailored to you.
13) Can I still exercise?
In many cases, yes—guided, gradual conditioning is helpful. We often recommend recumbent cardio early on, then build up as tolerance improves.
14) What outcomes do you track?
Symptoms, functional goals, Tytron scan patterns, alignment stability, and (if you choose) wearable metrics like HR/HRV and step counts.
15) How do I get started?
Call us at (941)243-3729 or visit www.chiropractorsarasotaflorida.com to schedule a complimentary consultation. We’ll review your history and determine whether upper cervical care is a good fit.
Your Next Step: A Calmer, More Capable Nervous System
Dysautonomia and POTS do not define you. With the right plan—and a team that understands the atlas–vagus connection—many patients regain steadiness, confidence, and momentum. At Lavender Family Chiropractic, we combine 3D CBCT, Tytron functional nervous system scans, and gentle upper cervical corrections to address a key control center of your physiology. If you’ve been searching for a “chiropractor Sarasota Florida,” “upper cervical chiropractor near me,” “Vertigo doctor near me,” or “Migraine doctor near me,” we’d be honored to help you explore this path.
Lavender Family Chiropractic in Sarasota Florida offers complimentary consultations to learn more about you. Click the link below!
https://intake.chirohd.com/new-patient-scheduling/724/lavender-family-chiropractic
Visit our Website!
To learn more about us go to http://www.chiropractorsarasotaflorida.com
We also service Bradenton, Parrish, Ellenton, Ruskin, Venice, Tampa, St. Pete, Osprey, Longboat, Lakewood Ranch, Myakka City.
If you are in Tampa, Fort Myers, or Salt Lake City, you can visit my other locations! NeckWise Upper Cervical. Visit, www.neckwise.com
If you are not local, visit www.uccnearme.com to find a doctor in your area.
Lavender Family Chiropractic
5899 Whitfield Ave Ste 107, Sarasota, FL 34243
Call: (941)243-3729
Web: www.chiropractorsarasotaflorida.com
Proudly serving: Sarasota, Bradenton, Lakewood Ranch, Parrish, Ellenton, Venice, Osprey, Punta Gorda, St. Petersburg, Siesta Key, Longboat Key, Lido Key, and Myakka City.
If you’re ready for an approach that treats you like a whole person—and respects the complexity of dysautonomia—schedule your complimentary consultation today. We’re here to help you feel steady, clear, and in control again.