Introduction
High blood pressure—clinically referred to as hypertension—affects nearly half of all adults in the United States, making it one of the most prevalent chronic health conditions today. Dubbed the “silent killer,” hypertension often progresses without noticeable symptoms yet significantly elevates the risk of heart attack, stroke, kidney disease, and even cognitive decline. According to the Centers for Disease Control and Prevention, only about one in four adults with hypertension has the condition under control, leading to substantial healthcare costs—estimated at over $131 billion annually in direct medical expenses and lost productivity.
At Lavender Family Chiropractic in Sarasota, Florida, our mission is to provide upper cervical chiropractic care that addresses the neurological and musculoskeletal root causes of autonomic dysregulation. By focusing on the precise alignment of the atlas (C1) and axis (C2) vertebrae, we help restore balanced communication between the brainstem and the cardiovascular system. In this comprehensive 3,500-word guide, we will explore:
- What constitutes hypertension, its risk factors, and complications
- The “silent” symptoms of elevated blood pressure and the importance of vigilant monitoring
- The landmark 2007 clinical trial demonstrating significant blood pressure reductions following atlas adjustments
- The neuro-anatomical connection between the upper cervical spine and the vasomotor nucleus in the brainstem
- Detailed anatomy of C1 and C2 and how misalignments occur
- Lavender Family Chiropractic’s evidence-based protocol: from functional nervous system scans to 3D CBCT imaging and the Knee-Chest technique
- Integrative lifestyle strategies—diet, exercise, stress management, sleep, and targeted supplements—to support natural blood pressure control
- Patient success stories and practice outcome data reinforcing the value of this approach
- Fifteen in-depth FAQs on hypertension and natural therapies
- Practical next steps for those considering upper cervical chiropractic care
1. Understanding Hypertension: Definitions, Risk Factors, and Complications
1.1 What Is Blood Pressure?
Blood pressure measures the force of circulating blood on arterial walls. It is recorded as two values:
- Systolic Pressure (Top Number): The pressure in arteries when the heart’s left ventricle contracts and ejects blood.
- Diastolic Pressure (Bottom Number): The pressure when the heart relaxes between beats, allowing chambers to refill.
A persistent elevation of either value defines hypertension.
1.2 Blood Pressure Categories (AHA Guidelines)
| Category | Systolic (mm Hg) | Diastolic (mm Hg) |
|---|---|---|
| Normal | < 120 | < 80 |
| Elevated | 120–129 | < 80 |
| Stage 1 Hypertension | 130–139 | 80–89 |
| Stage 2 Hypertension | ≥ 140 | ≥ 90 |
According to a 2023 report, almost 48% of American adults meet the criteria for Stage 1 or Stage 2 hypertension, yet up to 80% remain unaware or undertreated.
1.3 Key Risk Factors
Non-Modifiable Factors
- Genetics: A family history of hypertension doubles your lifetime risk.
- Age: Vascular stiffness and endothelial changes raise pressure as you age—especially after 45 in men and after 55 in women.
- Ethnicity: African-American adults face higher hypertension rates and more severe complications.
Modifiable Factors
- Dietary Sodium Excess: The average U.S. adult consumes over 3,400 mg of sodium daily, far above the recommended < 2,300 mg.
- Potassium Deficiency: Adequate potassium (≥ 4,700 mg/day) helps counteract sodium’s effects.
- Sedentary Lifestyle: Fewer than 25% of adults meet the guideline of ≥ 150 minutes/week of moderate-intensity activity.
- Obesity: Each 22-pound increase in body weight can raise systolic pressure by 1 mm Hg.
- Chronic Stress: Elevated cortisol and catecholamines trigger vasoconstriction and cardiac workload.
- Alcohol & Tobacco: Both induce endothelial dysfunction and sympathetic overactivity.
1.4 Complications of Uncontrolled Hypertension
- Cardiovascular Disease: Left ventricular hypertrophy, coronary artery disease, and heart failure.
- Cerebrovascular Events: Increased risk of ischemic and hemorrhagic stroke.
- Chronic Kidney Disease: Hypertensive nephropathy often progresses to end-stage renal failure.
- Retinopathy: Damage to retinal vessels can lead to vision loss.
- Cognitive Decline: Vascular dementia and Alzheimer’s risk increase with long-standing hypertension.
- Peripheral Artery Disease: Claudication and poor wound healing in the extremities.
Effective management requires a multi-pronged approach—addressing both conventional medical interventions and complementary therapies like upper cervical chiropractic care to mitigate neurological contributors.
2. Recognizing the “Silent” Symptoms of Hypertension
Hypertension is notorious for progressing without overt warning signs. However, some individuals may notice:
- Morning Headaches: Resulting from nocturnal blood pressure spikes.
- Persistent Fatigue or Brain Fog: Due to subtle cerebrovascular changes.
- Lightheadedness or Dizziness: Indicative of fluctuating perfusion.
- Blurred Vision: Hypertensive retinopathy can temporarily impair sight.
- Nocturia (Frequent Nighttime Urination): Linked to renal pressure changes.
- Palpitations or Chest Tightness: May occur during exertion.
- Epistaxis (Nosebleeds): Rare but can signal dangerously high readings (> 180/120 mm Hg).
2.1 Importance of Routine Monitoring
Because symptoms are unreliable, regular screening is vital:
- In-Office Checks: At least twice yearly for adults without risk factors; quarterly for those with pre-hypertension or higher.
- Home Monitoring: Use a validated, cuff-style device. Record readings twice daily—morning and evening—for one week every month.
- Ambulatory Blood Pressure Monitoring (ABPM): A 24-hour device can differentiate “white-coat” from true hypertension.
3. The 2007 Atlas Adjustment Study: A Paradigm Shift
In 2007, Dr. George Bakris et al. published a randomized, double-blinded trial in the Journal of Human Hypertension examining atlas (C1) realignment in hypertensive patients already on stable medications. Key elements:
- Sample: 50 adults with Stage 1 or Stage 2 hypertension, on one or two antihypertensive drugs for at least six months.
- Methods:
- Intervention Group (n=25): Received a precise atlas adjustment via the Knee-Chest upper cervical technique.
- Sham Group (n=25): Underwent a simulated procedure without therapeutic force.
- Outcomes:
- Mean systolic reduction: 14 mm Hg
- Mean diastolic reduction: 8 mm Hg
- Duration of effect: Sustained at eight-week follow-up
These findings paralleled the effect of adding a second pharmaceutical agent, suggesting that correcting atlas misalignment modulates autonomic tone and vascular resistance. This landmark study opened avenues for non-pharmacological management of hypertension.
4. Neuro-Anatomical Connection: Upper Cervical Spine & Blood Pressure Regulation
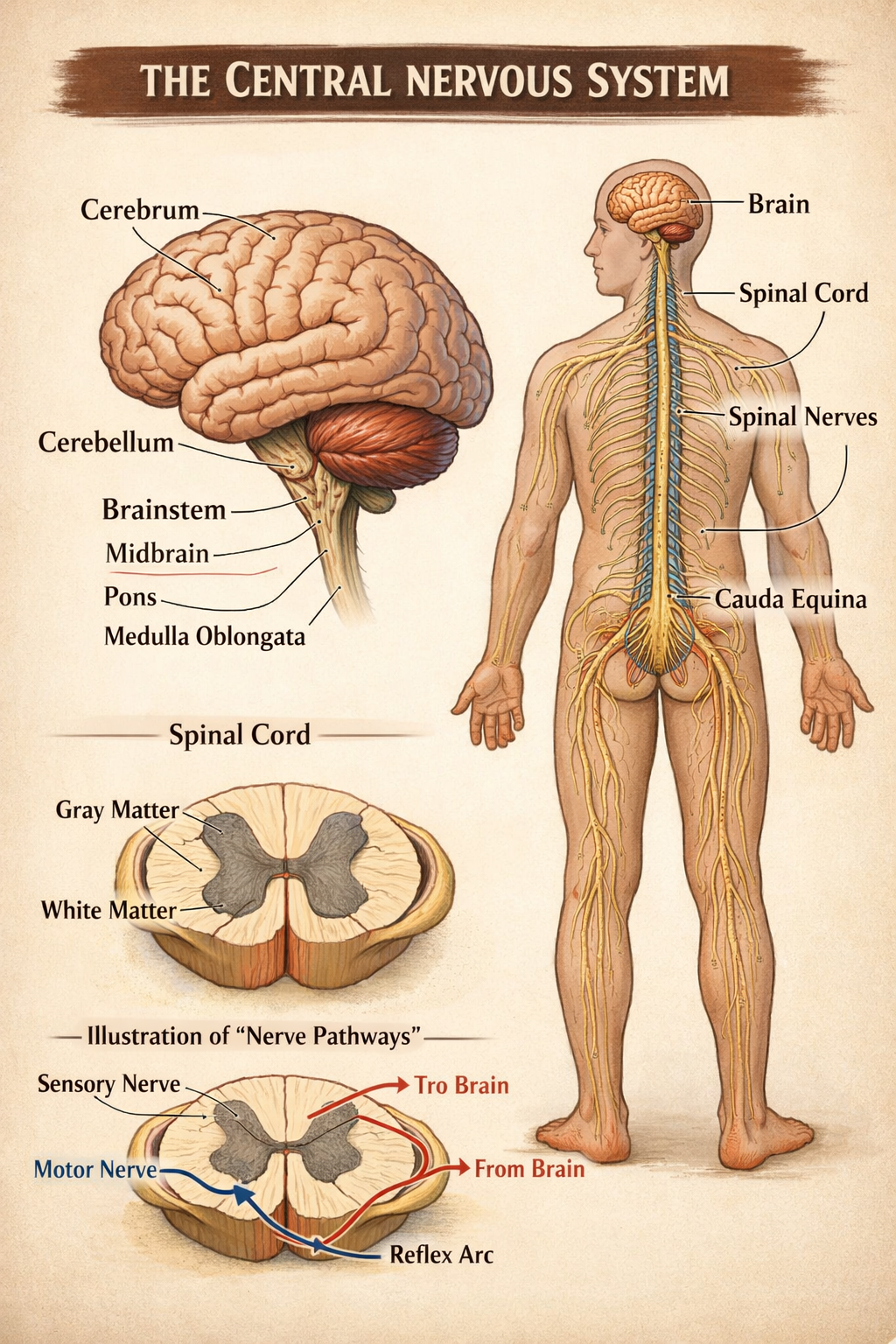
4.1 The Brainstem’s Vasomotor Center
Deep within the medulla oblongata lies the rostral ventrolateral medulla (RVLM)—the primary vasomotor nucleus:
- Inputs: Baroreceptors in the carotid sinus and aortic arch relay blood pressure changes. Chemoreceptors monitor blood gas levels.
- Outputs: Efferent sympathetic fibers descend to the intermediolateral cell column in the spinal cord, controlling vascular smooth muscle tone.
Balanced RVLM activity maintains homeostatic blood pressure. Perturbations shift the setpoint toward higher sympathetic drive and vasoconstriction.
4.2 Vagus Nerve and Parasympathetic Balance
Opposing the RVLM’s sympathetic outflow, the dorsal motor nucleus of the vagus modulates heart rate via parasympathetic efferents. A harmonious interplay between these two nuclei ensures stable cardiovascular dynamics.
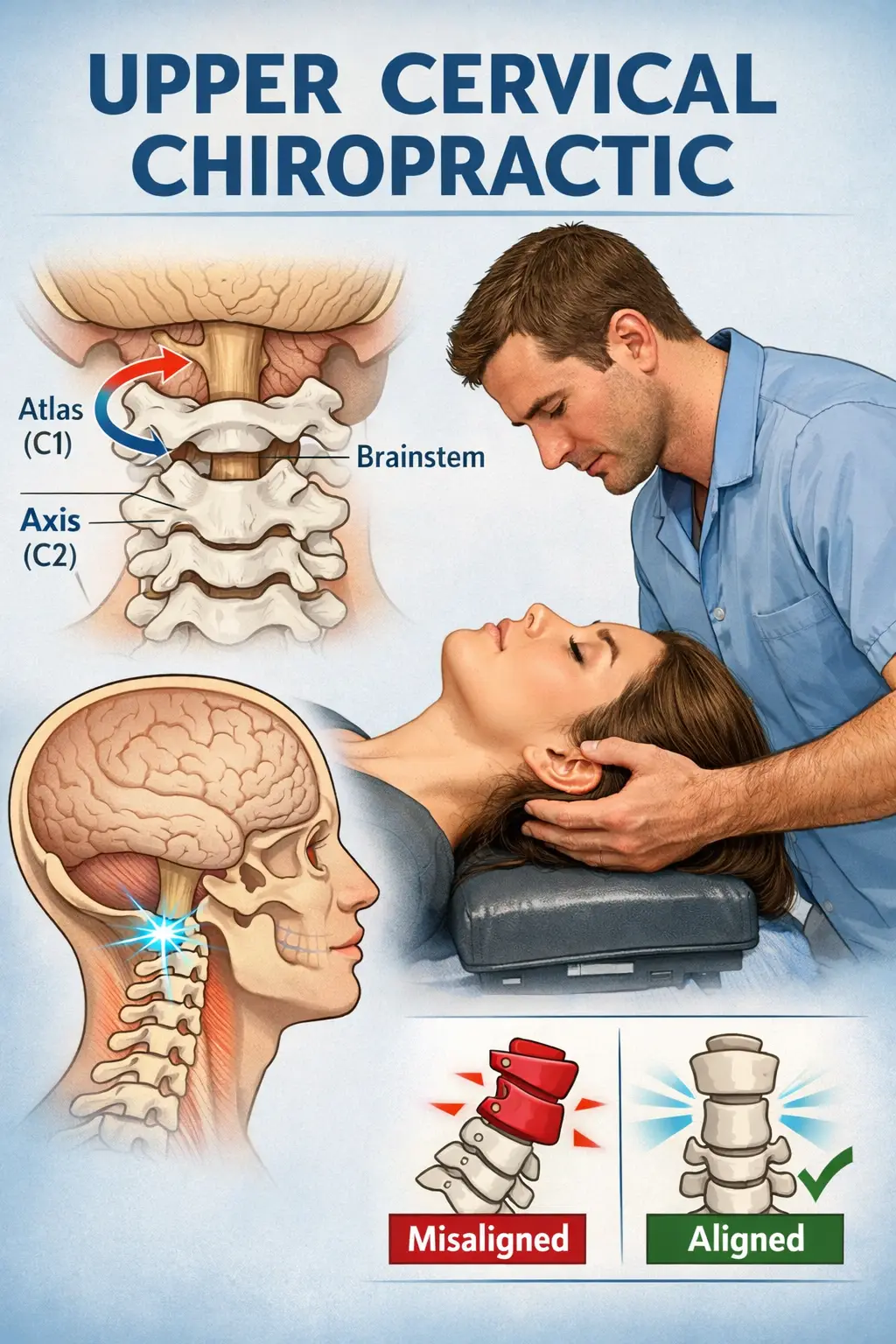
4.3 How Atlas Misalignments Disrupt Autonomic Equilibrium
- Mechanical Stress to the Foramen Magnum: Even sub-millimeter shifts in the atlas can distort the space where the brainstem resides, impinging on critical autonomic centers.
- Alteration in CSF Flow: Misalignment may impede cerebrospinal fluid pulsations, leading to slight intracranial pressure variations that trigger sympathetic reflexes.
- Vertebral Artery Tension: C1/C2 misplacement can kink vertebral arteries, reducing posterior circulation and eliciting compensatory vasoconstriction.
- Proprioceptive Mismatch: Abnormal mechanoreceptor firing in the upper cervical joint capsules sends distorted signals to central autonomic networks, accentuating “fight-or-flight” responses.
By correcting the alignment, upper cervical chiropractic care aims to normalize these pathways—reducing sympathetic overdrive and enhancing parasympathetic tone.
5. In-Depth Cervical Anatomy: Atlas, Axis, and Supporting Structures
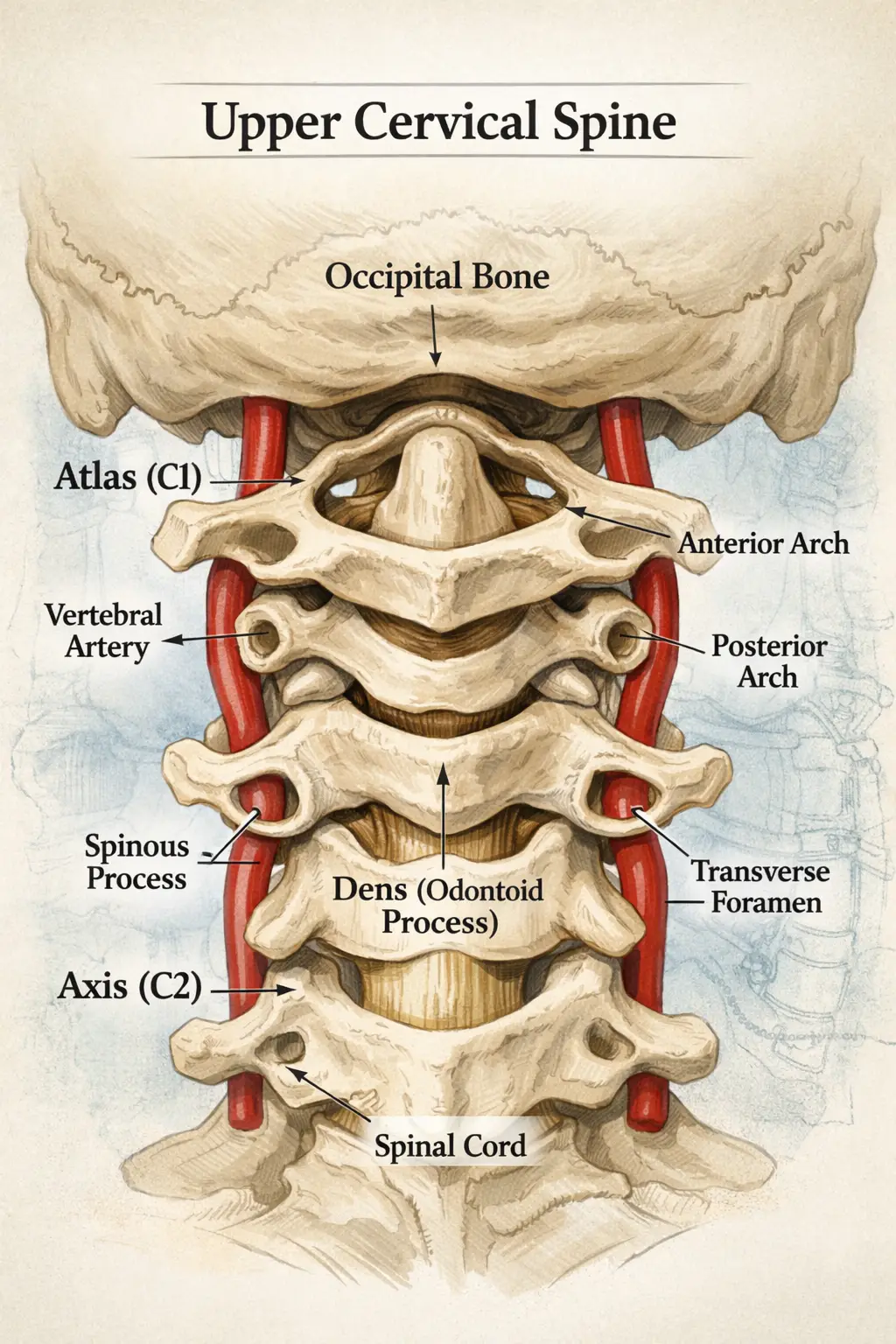
5.1 Atlas (C1)
- Structure: Ring-shaped vertebra without a vertebral body, articulating directly with the occiput.
- Function: Facilitates nodding (“yes”) through the atlanto-occipital joint.
- Unique Features: Anterior and posterior arches, lateral masses bearing the weight of the skull.
5.2 Axis (C2)
- Dens (Odontoid Process): A peg-like projection around which C1 pivots, enabling rotation (“no”).
- Atlanto-Axial Joint: Contributes to 50% of cervical rotation range of motion.
5.3 Ligamentous and Membranous Support
- Transverse Ligament: Secures the dens against the anterior arch of C1, preventing posterior displacement.
- Alar Ligaments: Limit excessive rotation by connecting the dens to the occipital condyles.
- Tectorial Membrane: A continuation of the posterior longitudinal ligament, reinforcing the spinal canal roof.
- Ligamentum Nuchae: Provides midline stabilization and rich proprioceptive input.
Minor deviations in this region can cascade into significant neurological and vascular disturbances.
6. Lavender Family Chiropractic’s Evidence-Based Protocol
6.1 Comprehensive Initial Evaluation
- Medical History & Symptom Review: Detailed questionnaire focusing on cardiovascular health, headaches, balance issues, and stress levels.
- Digital Posture Analysis: High-resolution photographs assess head-to-torso alignment and identify compensatory patterns.
- Thermal Scan (Infrared Thermography): Detects temperature asymmetries along paraspinal nerves indicative of autonomic imbalances.
- VSC Neural Scan (Galvanic Skin Response): Measures skin conductance differentials to localize sympathetic hyperactivity.
6.2 Advanced Imaging with 3D CBCT
- Cone-Beam CT Technology: Captures a three-dimensional view of the cranio-cervical complex, precisely measuring atlas rotation, lateral tilt, and anterior/posterior translations.
- Low Radiation Dose: Ensures patient safety while providing detailed anatomical insights—crucial when standard X-rays lack the resolution to detect subtle misalignments.
6.3 The Knee-Chest Upper Cervical Adjustment Technique
- Patient Positioning: The patient lies prone with hips and knees flexed, reducing lumbar lordosis and isolating C1–C2.
- Practitioner Contact: A refined, finger-tip contact on a specific atlas landmark.
- Force Application: A calibrated, low-force impulse—often imperceptible to the patient—corrects multi-planar misalignments without cavitation (“cracking”).
- Safety: This method minimizes joint stress and is exceptionally well-tolerated, even by those with osteoporosis or acute pain.
6.4 Immediate and Long-Term Monitoring
- Post-Adjustment Scans: Repeat thermal and VSC scans confirm reductions in autonomic dysregulation.
- Blood Pressure Re-Check: In-office measurement tracks acute changes, guiding treatment frequency.
- Home Protocols:
- Gentle Postural Exercises: Chin-tucks, corner stretches, and scapular retractions reinforce alignment.
- Hydration & Electrolyte Balance: Adequate water intake and minerals support vascular tone.
- Sleep Hygiene: Strategies for deep, restorative sleep to facilitate neurological repair.
6.5 Treatment Phases
- Correction Phase: 3–4 visits over two weeks to establish initial alignment and observe acute neurological responses.
- Stabilization Phase: Weekly adjustments for 4–6 weeks to maintain alignment and support lasting autonomic changes.
- Maintenance Phase: Bi-monthly to quarterly check-ups, based on individual goal—often synchronized with routine primary care visits.
7. Integrative Natural Strategies to Complement Upper Cervical Care
While upper cervical adjustments address neurological drivers of hypertension, combining them with lifestyle interventions amplifies and sustains blood pressure reductions.
7.1 Dietary Approaches
- DASH Diet (Dietary Approaches to Stop Hypertension):
- Key Components: Fruits, vegetables, low-fat dairy, whole grains, lean proteins, nuts, and legumes.
- Sodium Limit: ≤ 1,500 mg/day for those with hypertension.
- Potassium Focus: ≥ 4,700 mg/day from natural sources (bananas, spinach, sweet potatoes).
- Mediterranean Diet Elements:
- Healthy Fats: Extra-virgin olive oil, avocados, and fatty fish rich in omega-3s.
- Antioxidant-Rich Foods: Berries, dark leafy greens, tomatoes, and red grapes.
- Anti-Inflammatory Spices & Herbs: Turmeric, ginger, garlic, and green tea help mitigate vascular inflammation.
7.2 Exercise Recommendations
- Aerobic Activity:
- Goal: ≥ 150 minutes/week of moderate intensity (brisk walking, swimming, cycling).
- Benefit: Can lower systolic pressure by up to 8–10 mm Hg.
- Resistance Training:
- Frequency: 2–3 sessions/week, focusing on major muscle groups.
- Effect: Contributes an additional 4–5 mm Hg reduction.
- Mind-Body Exercises:
- Yoga & Tai Chi: Combine physical movement with breath control—shown to reduce resting blood pressure by 5–7 mm Hg.
7.3 Stress Management Techniques
- Diaphragmatic (“Belly”) Breathing:
- Practice: 5–10 minutes/day, inhaling deeply to expand the abdomen and exhaling fully to activate the parasympathetic nervous system.
- Progressive Muscle Relaxation:
- Method: Systematically tense and relax major muscle groups, focusing on release of tension.
- Guided Imagery & Meditation:
- Tools: Smartphone apps (e.g., Insight Timer, Headspace) for daily 10–20 minute sessions.
- Biofeedback:
- Use: Real-time feedback on heart rate variability to train autonomic self-regulation.
7.4 Sleep & Recovery
- Sleep Duration: 7–9 hours/night reduces cortisol levels and supports endothelial repair.
- Sleep Environment: Cool, dark, and quiet; avoid screens and stimulants (caffeine, nicotine) 2–3 hours before bed.
- Routine: Consistent bedtime and wake time—even on weekends—to reinforce circadian rhythms.
7.5 Targeted Nutritional Supplements** (Under Professional Guidance)
| Supplement | Typical Dosage | Potential Effect |
|---|---|---|
| Coenzyme Q10 | 100–200 mg/day | May reduce systolic by ~11 mm Hg |
| Magnesium (Citrate or Glycinate) | 300–400 mg/day | Supports vascular smooth muscle relaxation |
| Omega-3 Fatty Acids | 1,000–2,000 mg EPA/DHA | Anti-inflammatory, improves endothelial function |
| Potassium | 1,500–4,700 mg/day | Balances sodium, reduces vascular resistance |
| Vitamin D | 1,000–2,000 IU/day | Deficiency linked to hypertension |
Always consult a qualified healthcare provider before initiating supplements—especially if you’re on medications.
8. Patient Success Stories & Practice Outcome Data
Real-world outcomes from Lavender Family Chiropractic underscore the transformative impact of combining upper cervical care with integrative strategies:
| Patient | Baseline BP (mm Hg) | Post-Care BP | Timeframe | Notes |
|---|---|---|---|---|
| Maria S. | 142/88 | 124/76 | 8 weeks | Eliminated one medication; reported improved sleep and reduced headaches |
| James R. | 150/92 | 130/80 | 2 months | Reduced two med dosages; energy levels markedly increased |
| Angela T. | 138/84 | 122/74 | 6 weeks | Noted decreased anxiety, better focus at work |
| Michael L. | 160/96 | 136/82 | 10 weeks | Paired upper cervical care with DASH diet; no new meds needed |
| Linda P. | 145/89 | 128/78 | 12 weeks | Experienced fewer migraine days and improved quality of life |
| Daniel K. | 152/94 | 132/82 | 8 weeks | Reported better exercise tolerance and reduced palpitations |
These outcomes mirror the Bakris study, illustrating that precise atlas correction can deliver clinically significant reductions—often rivaling pharmaceutical interventions.
9. Fifteen In-Depth FAQs About Hypertension & Natural Treatment
- What makes upper cervical chiropractic different from traditional chiropractic?
Upper cervical focuses exclusively on the C1–C2 region using low-force, highly specific adjustments—no full-spine manipulation or high-velocity thrusts. - How can a misalignment so high in the neck affect blood pressure?
The atlas surrounds the foramen magnum, where the brainstem and vasomotor nucleus reside. Misalignment irritates autonomic centers, increasing sympathetic drive. - Is the atlas adjustment painful or risky?
No—the Knee-Chest technique uses minimal force and is considered among the safest chiropractic methods, even for patients with osteoporosis or acute injury. - How quickly will I see improvements in blood pressure?
Some patients notice reductions within days; most see significant, sustained changes after 4–8 weeks of care combined with lifestyle modifications. - Will my primary care doctor support this approach?
Many progressive physicians recognize the role of autonomic regulation. We encourage collaborative care, sharing reports and imaging results. - Can I reduce or stop my blood pressure medications?
Any medication changes should occur under your physician’s supervision. Several of our patients successfully taper doses after achieving stable readings. - What lifestyle changes should accompany chiropractic?
A DASH-style diet, regular aerobic and resistance exercise, stress management (meditation, breathing), quality sleep, and targeted supplementation. - How frequently should I receive adjustments for hypertension?
Typically, an initial correction phase of 3–4 visits in 2 weeks, followed by weekly stabilization visits for 4–6 weeks, then maintenance every 1–3 months. - Are there contraindications to upper cervical chiropractic?
Severe vertebral artery disease, certain connective tissue disorders, or acute trauma may require medical clearance. Our comprehensive evaluation identifies any red flags. - Does insurance cover upper cervical care?
Many major insurers cover chiropractic; coverage for upper cervical techniques varies. Our administrative team assists with benefit verification and superbills. - Can children and adolescents with hypertension benefit?
Yes—gentle upper cervical assessments can support autonomic balance in pediatric and adolescent populations under proper medical supervision. - What at-home exercises support cervical alignment?
Chin Tucks, Wall Angels, Corner Stretches, and Scapular Squeezes—5–10 minutes daily to reinforce postural corrections. - How does stress exacerbate hypertension?
Chronic stress elevates cortisol and catecholamines, driving vasoconstriction, sodium retention, and increased cardiac output. - What is the role of the vagus nerve in blood pressure control?
Vagal tone mediates parasympathetic effects—slowing heart rate and promoting vasodilation. Balanced brainstem function enhances vagal activity. - How do I get started at Lavender Family Chiropractic?
Call us ator visit www.chiropractorsarasotaflorida.com to book your Comprehensive Upper Cervical Evaluation, including digital scans and 3D CBCT imaging. We’ll design a personalized plan to help you achieve and maintain optimal blood pressure.(941) 243-3729
10. Practical Next Steps & Call to Action
- Schedule Your Initial Evaluation: Early detection of atlas misalignment is key—don’t wait for complications to emerge.
- Begin Home Monitoring: Invest in a validated home blood pressure monitor and keep a log of daily readings.
- Adopt the DASH Principles: Start incorporating more fruits, vegetables, whole grains, and lean proteins into every meal.
- Incorporate Stress-Reduction Practices: Even 5 minutes of diaphragmatic breathing daily can shift autonomic balance.
- Stay Active: Aim for at least 30 minutes of moderate exercise most days to support vascular health.
At Lavender Family Chiropractic, we’re committed to providing a professional yet personal experience—guiding you through every step, from cutting-edge imaging and gentle adjustments to lifestyle coaching and follow-up care. By addressing the neurological root of hypertension and empowering you with evidence-based natural strategies, we help you reclaim your cardiovascular health—without over-reliance on medications or invasive procedures.
Conclusion
Hypertension management is evolving beyond pills and protocols. Upper cervical chiropractic care—anchored in scientific inquiry and precise correction of atlas misalignment—offers a novel, drug-free pathway to reduce blood pressure, mitigate autonomic stress, and enhance overall well-being. When combined with DASH-style nutrition, regular exercise, stress management, and quality sleep, this integrated model can rival conventional multi-drug regimens, often with fewer side effects and greater improvements in patient quality of life.
If you’re ready to explore how upper cervical chiropractic can complement your existing care plan, contact Lavender Family Chiropractic today. Our Sarasota team is here to support you in achieving stable, natural blood pressure control—one gentle adjustment at a time.
Schedule With Us!
Lavender Family Chiropractic in Sarasota Florida offers complimentary consultations to learn more about you. Click the link below!
https://intake.chirohd.com/new-patient-scheduling/724/lavender-family-chiropractic
Visit our Website!
To learn more about us go to http://www.chiropractorsarasotaflorida.com
We also service Bradenton, Parrish, Ellenton, Ruskin, Venice, Tampa, St. Pete, Osprey, Longboat, Lakewood Ranch, Myakka City.
If you are not local, visit www.uccnearme.com to find a doctor in your area!