Persistent Postural-Perceptual Dizziness (PPPD) is one of the most misunderstood and frustrating balance disorders people experience. Many individuals with PPPD describe feeling constantly off-balance, lightheaded, foggy, or disconnected from their surroundings, even when standard medical testing comes back normal. For some, the symptoms are mild but persistent. For others, PPPD is completely life-altering—affecting work, driving, social activities, and emotional well-being.
At Lavender Family Chiropractic – NeckWise North Sarasota, serving Sarasota and Lakewood Ranch, Florida, we see a consistent pattern: PPPD is very often not just an inner ear or anxiety issue—it is frequently a neck-related neurological imbalance, rooted in dysfunction of the upper cervical spine and the way the brain processes balance.
What Is Persistent Postural-Perceptual Dizziness (PPPD)?
Persistent Postural-Perceptual Dizziness (PPPD) is a chronic disorder of balance perception and neurological processing rather than a disease of the inner ear alone. People with PPPD experience ongoing sensations of dizziness, imbalance, rocking, swaying, or lightheadedness that persist for at least three months and often much longer.
Unlike classic vertigo, PPPD does not typically cause a spinning sensation. Instead, individuals feel as though their body or the environment is subtly moving, unstable, or disconnected. Many describe the sensation as being on a boat, walking on foam, or feeling slightly pulled or tilted even while standing still.
PPPD is considered a functional neurological condition, meaning the structure of the brain and inner ears may appear normal on imaging, but the way the nervous system processes balance information is altered. This is why so many people feel invalidated or dismissed during the diagnostic process.
PPPD commonly begins after an initial trigger such as an episode of vertigo, vestibular neuritis, benign paroxysmal positional vertigo (BPPV), a concussion, whiplash injury, fall, illness, or significant emotional stress. In many cases, the original event resolves, but the nervous system remains locked into an abnormal balance strategy. The body adapts incorrectly and never fully resets.
This lingering neurological imbalance is where PPPD becomes chronic and where addressing only the inner ear or anxiety fails to fully resolve symptoms.
Why PPPD Is Often Misdiagnosed
PPPD is frequently misunderstood because it does not follow the rules of traditional vestibular disorders. Many patients undergo extensive testing including MRIs, CT scans, blood work, hearing tests, and vestibular exams, only to be told that everything looks normal. This disconnect between symptoms and test results can be deeply frustrating.
One reason PPPD is misdiagnosed is that most standard tests evaluate structural damage or inner ear pathology. PPPD, however, is a problem of neurological communication and sensory integration. The brain is receiving conflicting information about balance and posture and responds by staying in a constant state of vigilance.
Another reason PPPD is often labeled as anxiety is because the symptoms themselves can provoke fear. Feeling unsteady triggers the brain’s threat response, which can increase heart rate, muscle tension, and visual sensitivity. Over time, the body begins to associate movement and upright posture with danger.
While anxiety can absolutely amplify PPPD symptoms, it is not the root cause. The underlying issue is faulty balance signaling, very often influenced by dysfunction in the upper cervical spine and its connection to the brainstem.
Understanding this distinction is critical, because treating anxiety alone does not correct the mechanical and neurological dysfunction driving PPPD.
How Balance Is Processed in the Body
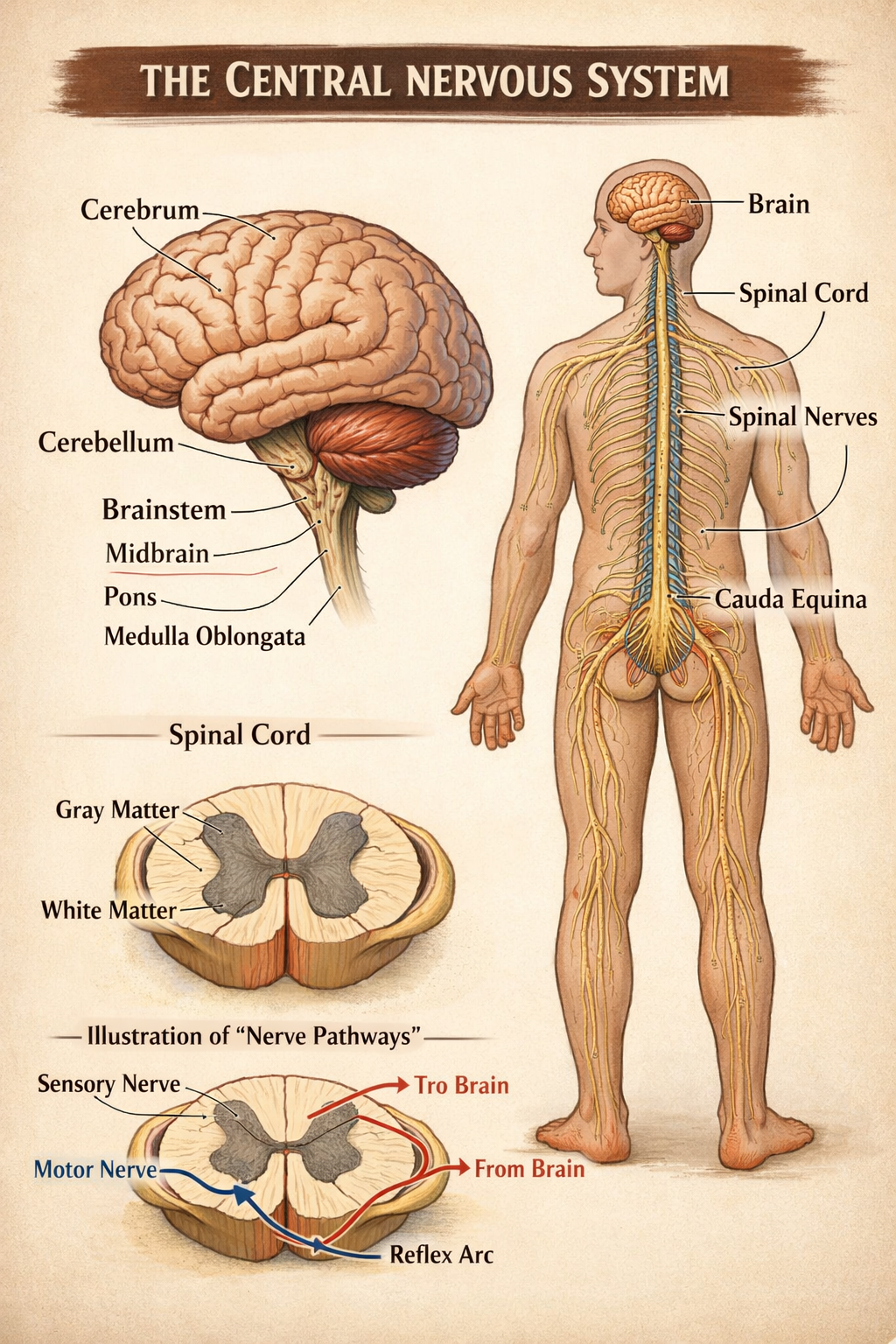
Balance is far more complex than most people realize. It is not controlled by a single organ or system but instead relies on constant communication between multiple sensory inputs that must be accurately integrated by the brain.
There are three primary balance systems:
The vestibular system, located in the inner ear, detects head movement and acceleration.
The visual system provides spatial orientation by interpreting movement and environmental reference points.
The proprioceptive system sends information from muscles, joints, and ligaments to tell the brain where the body is in space.
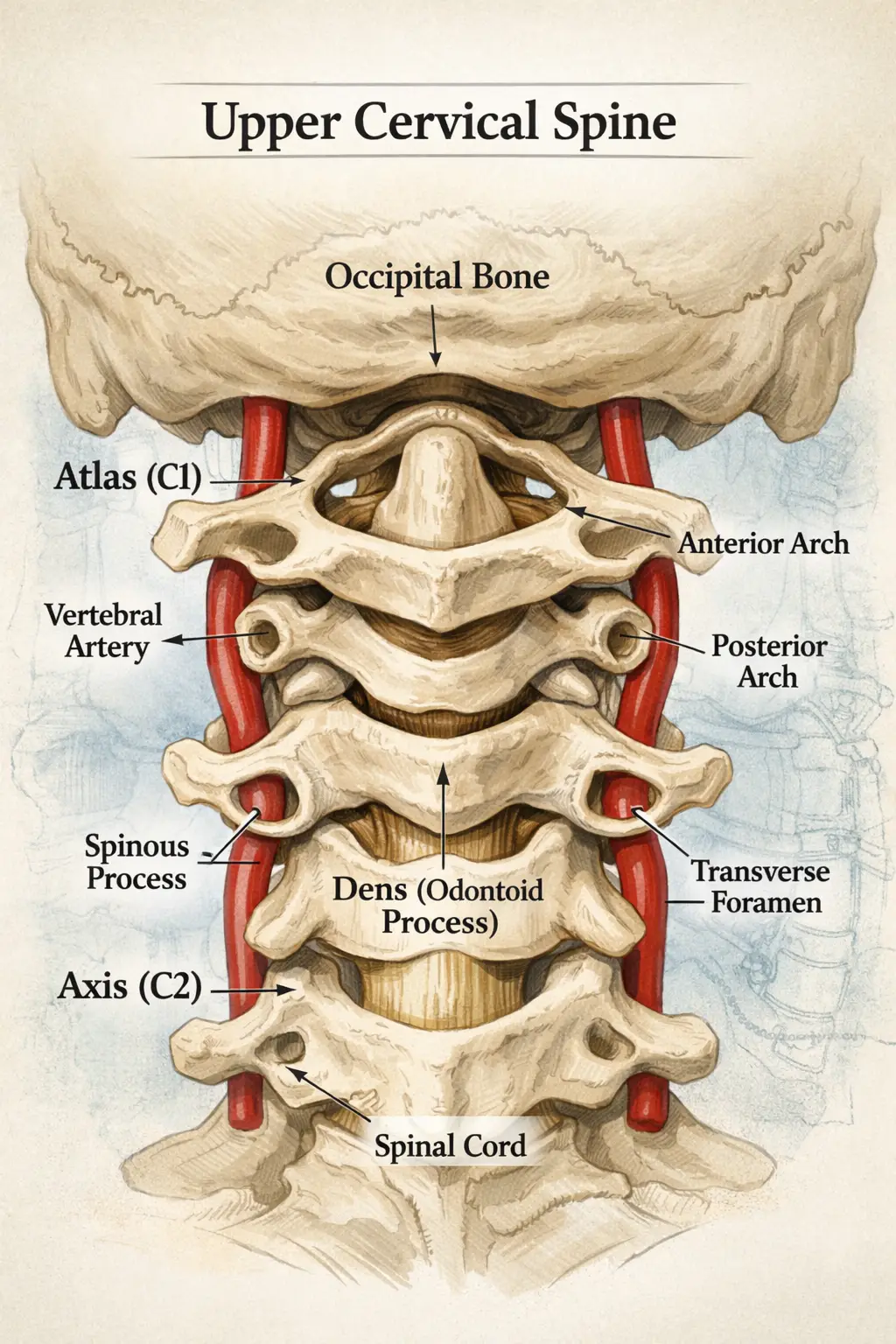
The upper cervical spine plays a uniquely important role in proprioception. The joints between the skull, atlas (C1), and axis (C2) contain one of the highest densities of proprioceptive receptors in the entire body. These receptors provide real-time feedback about head position, motion, and alignment.
This information travels directly to the brainstem, which acts as the command center for balance integration. When all three systems provide consistent information, balance feels effortless and automatic.
When one system provides distorted input, particularly from the upper cervical spine, the brain struggles to reconcile the conflicting data. The result is dizziness, unsteadiness, visual discomfort, and postural instability—hallmark features of PPPD.
The Upper Cervical Spine and PPPD
The upper cervical spine consists of the atlas (C1) and axis (C2), which support the head and protect the brainstem and upper spinal cord. This region is responsible for fine motor control, head orientation, and neurological signaling critical to balance and posture.
Because of its mobility and anatomical importance, the upper cervical spine is particularly vulnerable to injury. Even minor trauma such as low-speed car accidents, falls, sports injuries, or repetitive postural stress can cause subtle misalignments.
When the atlas or axis becomes misaligned, several problems can occur simultaneously. Proprioceptive input from the neck becomes distorted, sending inaccurate signals to the brain. Muscle tension patterns change, creating asymmetry and instability. Brainstem function may be irritated due to mechanical stress or altered neurological input.
In people with PPPD, this creates a perfect storm. The brain receives unreliable balance information from the neck and compensates by becoming hyper-aware of posture and movement. Over time, this hypervigilance becomes the new normal.
This is why PPPD is so often associated with neck pain, stiffness, headaches, jaw tension, visual sensitivity, and fatigue. The condition is not isolated to the inner ear; it is deeply rooted in upper cervical dysfunction.
Why PPPD Symptoms Persist
One of the most confusing aspects of PPPD is why symptoms continue long after the original trigger has resolved. From a neurological standpoint, the brain adapts to whatever sensory input it receives consistently, even if that input is incorrect.
When faulty balance information continues to come from the upper cervical spine, the brain creates compensatory strategies to maintain stability. These strategies may initially be protective but eventually become maladaptive. The nervous system stays in a guarded state, constantly monitoring posture and movement.
Over time, this leads to increased sensitivity to motion, busy environments, and upright posture. The brain essentially loses trust in automatic balance processes and attempts to consciously control what should be subconscious.
Without correcting the source of distorted input, the nervous system has no reason to change its strategy. This is why symptom management alone often fails to create lasting resolution.
The Brainstem Connection
The brainstem is one of the most critical and sensitive areas of the nervous system. It integrates information related to balance, eye movement, posture, muscle tone, breathing, heart rate, and autonomic nervous system regulation.
The upper cervical spine sits directly beneath the brainstem. Misalignment in this region can alter the way sensory information is delivered and processed. This does not require severe compression or damage; even subtle mechanical stress can disrupt normal signaling.
When the brainstem is under constant sensory conflict, the body may respond with dizziness, visual disturbances, anxiety, fatigue, and difficulty concentrating. These symptoms are not imagined; they are the result of a nervous system operating under stress.
This explains why PPPD frequently overlaps with conditions such as migraines, post-concussion syndrome, TMJ dysfunction, dysautonomia, and chronic neck pain. All share a common denominator of brainstem involvement.
What Is NeckWise Upper Cervical Care?
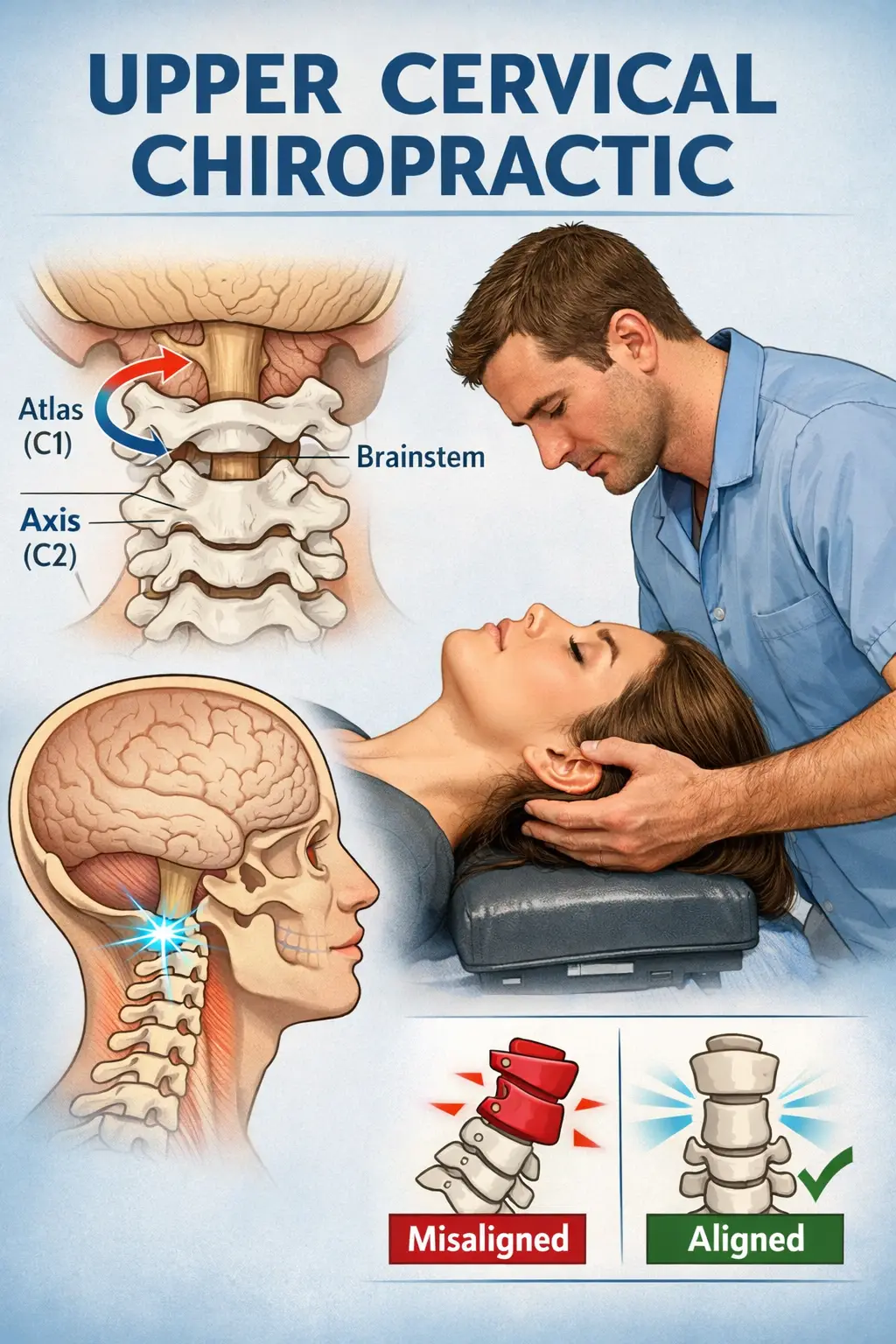
NeckWise upper cervical care is a highly specialized approach to chiropractic that focuses exclusively on the alignment and stability of the upper cervical spine. It is fundamentally different from traditional chiropractic methods.
Rather than adjusting the entire spine, NeckWise care concentrates on correcting the root structural imbalance at the top of the neck. This area has an outsized influence on neurological function and balance regulation.
Care begins with comprehensive assessment, including advanced 3D CBCT imaging. This imaging allows precise measurement of the position of the atlas and axis in three dimensions. No guesswork is involved.
Corrections are delivered gently and precisely, without twisting, cracking, or forceful manipulation. This makes NeckWise care especially appropriate for individuals with dizziness, PPPD, or sensitive nervous systems.
The goal is not repeated adjustments but long-term stability. When alignment is restored and maintained, the nervous system is finally able to recalibrate.
How NeckWise Care Helps PPPD
When upper cervical alignment is restored, the brain receives more accurate proprioceptive input from the neck. This improved communication allows the balance system to reorganize and normalize.
As neurological stress decreases, the brain becomes less reliant on protective balance strategies. Patients often notice gradual improvements in stability, confidence with movement, visual tolerance, and mental clarity.
NeckWise care does not force the nervous system to change. Instead, it removes interference and allows the body to heal naturally. This process takes time and consistency, but it addresses the root cause rather than masking symptoms.
Why Imaging Matters
Precision is essential when working with the upper cervical spine. Small misalignments can have large neurological consequences, especially in conditions like PPPD.
3D CBCT imaging provides a detailed view of joint alignment, angles, and structural integrity. This allows care to be customized to each individual rather than using generalized techniques.
By knowing exactly how the atlas and axis are positioned, corrections can be delivered safely and effectively, supporting long-term stability.
Why Choose Lavender Family Chiropractic – NeckWise North Sarasota
Lavender Family Chiropractic – NeckWise North Sarasota specializes in complex neurological and balance conditions. Our offices serving Sarasota and Lakewood Ranch focus on root-cause care for dizziness, PPPD, migraines, and post-concussion symptoms.
We take a calm, thorough, and patient-centered approach. Every case begins with listening, precise evaluation, and clear explanation. Care is never rushed, and progress is carefully monitored.
Our goal is not temporary relief but lasting neurological stability.
Hope for PPPD Patients
PPPD does not mean your body is broken. It means your nervous system has been stuck in a protective pattern. By addressing upper cervical alignment, the body can regain balance confidence and heal naturally.
Lavender Family Chiropractic – NeckWise North Sarasota is proud to serve Sarasota and Lakewood Ranch, Florida, helping patients find lasting relief from chronic dizziness and balance disorders.
Top 15 Frequently Asked Questions About Persistent Postural-Perceptual Dizziness (PPPD)
1. What does PPPD stand for?
PPPD stands for Persistent Postural-Perceptual Dizziness. It is a chronic neurological condition characterized by ongoing dizziness, unsteadiness, or non-spinning vertigo that lasts three months or longer.
2. Is PPPD a real medical condition?
Yes. PPPD is a recognized neurological diagnosis. While routine tests may appear normal, the condition involves altered balance processing within the brain and nervous system.
3. What does PPPD feel like?
Most people describe PPPD as rocking, swaying, lightheadedness, or feeling off-balance rather than spinning. Symptoms often worsen when standing, walking, or in visually busy environments.
4. What causes PPPD to start?
PPPD usually begins after an initial trigger such as vertigo, concussion, whiplash, illness, a fall, or a stressful event. The original issue may resolve, but the nervous system remains stuck in a dysfunctional balance pattern.
5. Is PPPD related to anxiety?
Anxiety can worsen PPPD symptoms, but it is not the root cause. PPPD involves faulty sensory integration and balance signaling, often influenced by the upper cervical spine and brainstem.
6. Can neck injuries cause or contribute to PPPD?
Yes. Neck injuries such as whiplash or concussions can disrupt proprioceptive input from the upper cervical spine, leading to abnormal balance processing and persistent dizziness.
7. Why are my tests normal if I feel so dizzy?
Standard imaging and vestibular tests often do not measure functional neurological imbalance. PPPD is a problem of sensory processing, not structural damage visible on routine scans.
8. Why do PPPD symptoms worsen when I’m upright or walking?
Being upright increases reliance on proprioceptive input from the neck and balance centers in the brainstem. If these signals are distorted, symptoms become more noticeable.
9. Can PPPD cause brain fog and fatigue?
Yes. PPPD often places the nervous system in a constant state of alert, which can lead to mental fatigue, difficulty concentrating, and brain fog.
10. How is PPPD usually treated?
Conventional approaches may include vestibular therapy or medication to manage symptoms. However, addressing upper cervical alignment can help correct the underlying neurological imbalance.
11. What is the connection between the upper cervical spine and balance?
The upper cervical spine contains a high concentration of balance receptors that communicate directly with the brainstem. Misalignment can distort balance signals sent to the brain.
12. Can upper cervical chiropractic care help PPPD?
Many people with PPPD improve when upper cervical misalignment is corrected. Proper alignment allows the brain to recalibrate balance processing naturally.
13. Is NeckWise care safe for people with dizziness?
Yes. NeckWise care uses gentle, precise corrections without twisting or cracking, making it well-suited for individuals with sensitive nervous systems.
14. How long does it take to see improvement with upper cervical care?
Every case is different. Some patients notice changes early, while others improve gradually as the nervous system stabilizes and adapts to correct alignment.
15. Can PPPD fully resolve?
Many people experience significant improvement or resolution when the root cause is addressed. Restoring proper neurological input from the upper cervical spine gives the body the best opportunity to heal.
Schedule a Consultation
If you’re searching for a chiropractor sarasota florida, chiropractor near me, upper cervical chiropractor near me, or you’ve been looking for answers to ear pressure, dizziness, vertigo, headaches, and chronic congestion, we’re here to help.
Lavender Family Chiropractic (NeckWise North Sarasota)
5899 Whitfield Ave Ste 107, Sarasota, FL 34243
www.chiropractorsarasotaflorida.com
(941)243-3729
To learn more about us go to http://www.chiropractorsarasotaflorida.com
We also service Bradenton, Parrish, Ellenton, Ruskin, Venice, Tampa, St. Pete, Osprey, Longboat, Lakewood Ranch, Myakka City.
If you are in Tampa, Land O Lakes, Fort Myers, or Salt Lake City, you can visit my other locations! NeckWise Upper Cervical. Visit, www.neckwise.com
If you are not local, visit www.uccnearme.com to find a doctor in your area
Serving Sarasota, Bradenton, Lakewood Ranch, Parrish, Ellenton, Venice, Osprey, Siesta Key, Longboat Key, Lido Key, Myakka City, Punta Gorda, and St. Petersburg.