Introduction
Post Concussion Syndrome: A concussion—even a “mild” one—can upend your life. While most people bounce back within a few weeks, an estimated 10–30% continue to experience symptoms well beyond three months. This lingering constellation of headaches, dizziness, brain fog, sleep disturbances, mood swings, and more is known as Post Concussion Syndrome (PCS). It can derail work, school, relationships, and the simple joy of everyday activities.
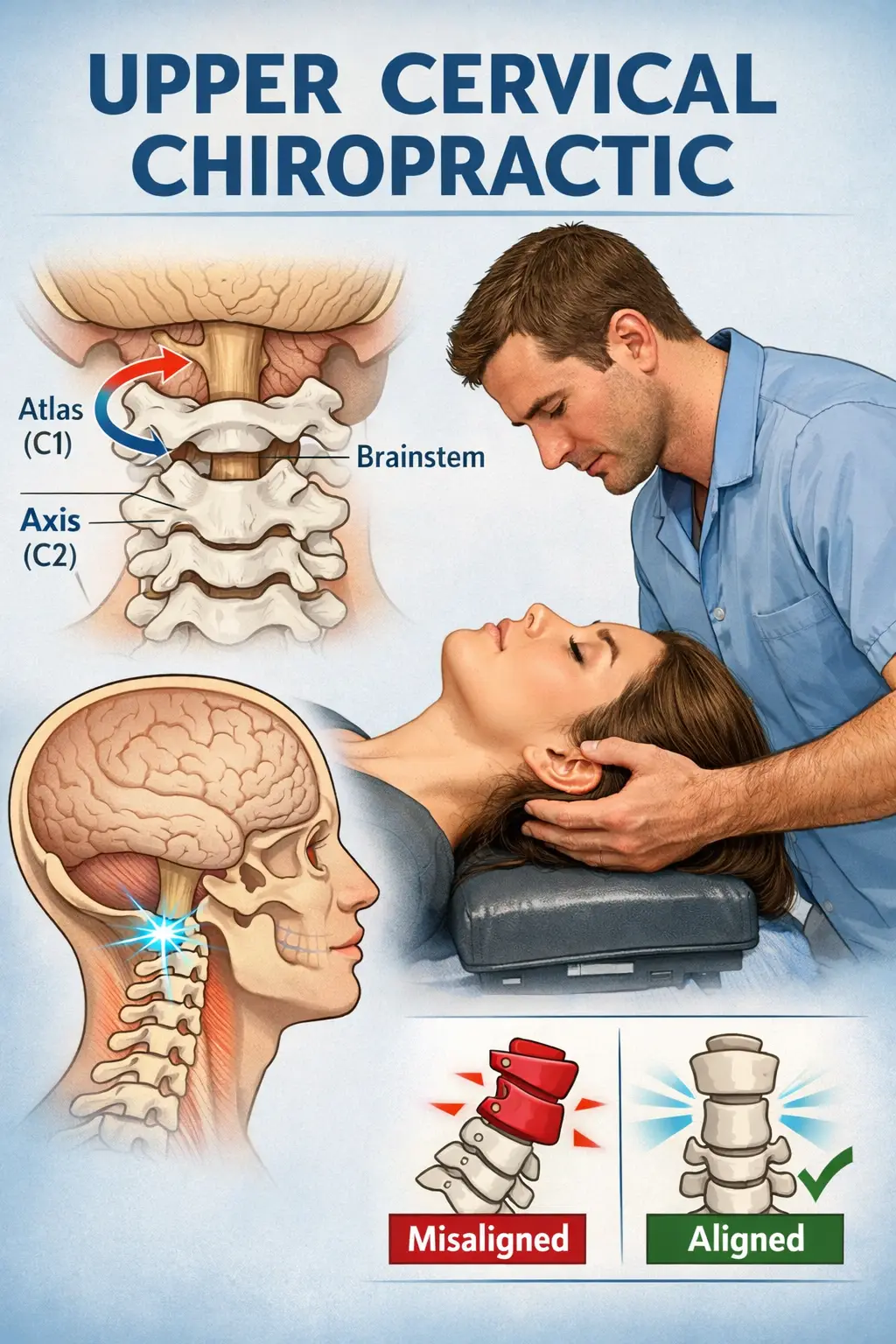
If you’re one of the many suffering from PCS, know there is hope. At Lavender Family Chiropractic, we specialize in upper cervical chiropractic care that addresses the root mechanical and neurological causes of PCS. Using state-of-the-art 3D CBCT X-ray imaging, paraspinal infrared thermography, and functional nervous system scans, we detect even sub-millimeter misalignments in your upper cervical spine (the atlas and axis vertebrae) that can impair brainstem function and cerebrospinal fluid flow. Our doctors then deliver gentle, hands-only adjustments, restoring proper alignment without twisting, popping, or cracking.
In this in-depth guide, you’ll learn:
- What causes PCS and why it lingers
- The common symptoms that derail daily life
- How upper cervical chiropractic differs from conventional care
- Lavender Family Chiropractic’s precise diagnostic protocols
- A typical treatment timeline
- Real patient success stories
- Cutting-edge research and case series
- Integrative rehabilitation and lifestyle recommendations
- Prevention and return-to-activity guidelines
- Pediatric and senior considerations
- Advanced technologies and multi-disciplinary approaches
- An expanded set of FAQs
- Actionable takeaways
By the end, you’ll understand why addressing your atlas alignment could be the missing link in your PCS recovery—and how to get started today.
What Causes Post Concussion Syndrome?
A concussion is a mild traumatic brain injury (mTBI) caused by a blow, bump, or jolt to the head or body that transmits force to the brain. Although called “mild,” the impact can trigger a cascade of physiological and neurological disturbances:
- Biomechanical Shear Injury
- Mechanism: Rapid acceleration–deceleration stretches axons (nerve fibers) within the brain’s white-matter tracts, causing micro-tears that disrupt neural communication pathways.
- Result: Impaired signaling leads to cognitive slowing, memory lapses, and brain fog.
- Inflammatory Cascade
- Mechanism: Release of cytokines and inflammatory mediators increases blood–brain barrier permeability, causing edema (swelling) and oxidative stress within neural tissues.
- Result: Prolonged inflammation maintains intracranial pressure imbalances, fueling persistent headaches and migraines.
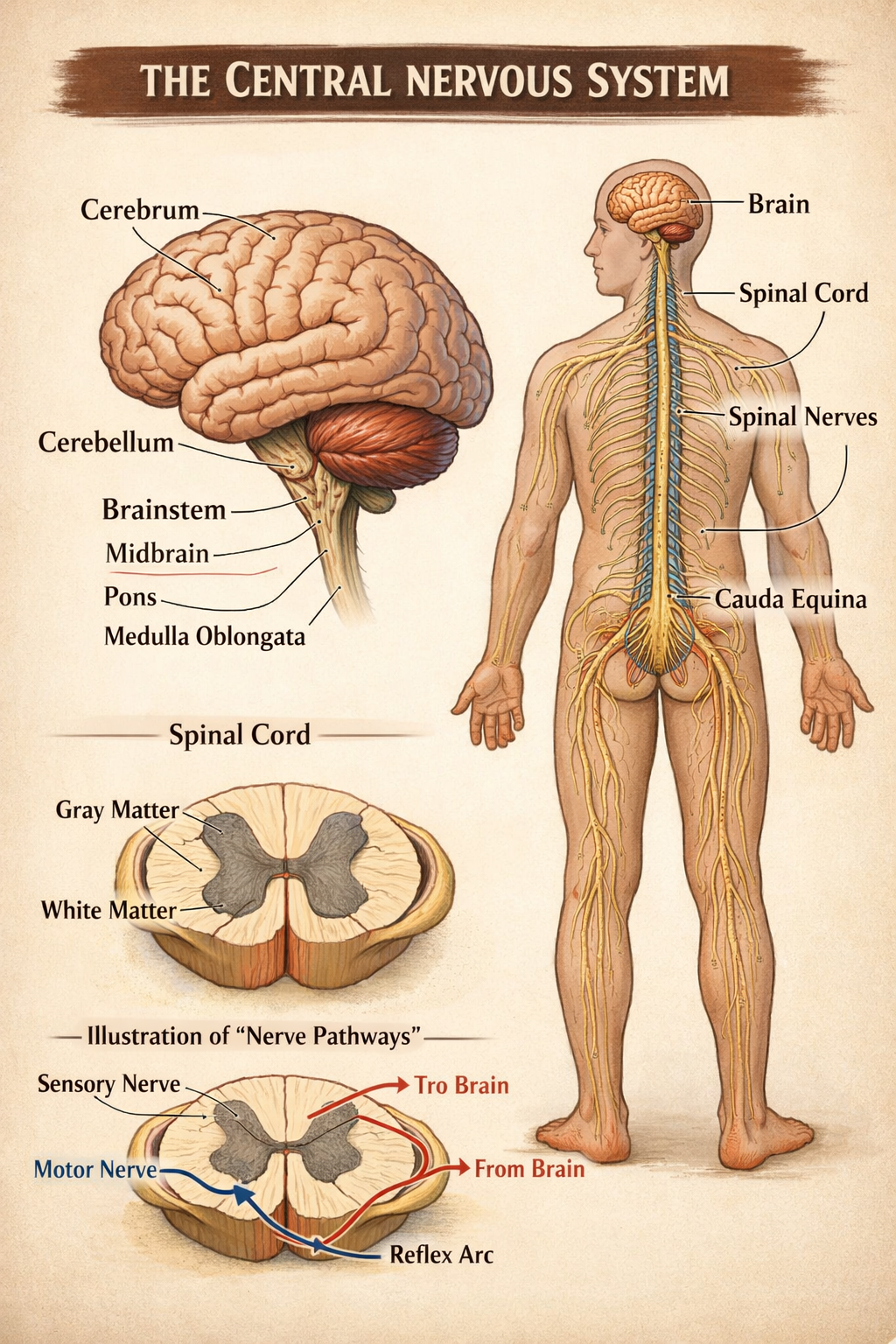
- Autonomic Nervous System (ANS) Dysregulation
- Mechanism: Concussion can dysregulate the balance between the sympathetic (“fight or flight”) and parasympathetic (“rest and digest”) branches of the ANS.
- Result: Fluctuating heart rate, blood-pressure spikes, sleep disturbances, and emotional lability (anxiety, irritability).
- Cerebrospinal Fluid (CSF) Flow Impedance
- Mechanism: Subtle misalignments of the atlas (C1) and axis (C2) vertebrae can obstruct CSF circulation around the brain and spinal cord.
- Result: Impaired nutrient exchange and waste removal perpetuate elevated intracranial pressure and lethargy.
- Secondary Musculoskeletal Effects
- Mechanism: Protective muscle guarding and altered posture post-injury increase tension in the neck, shoulders, and upper back.
- Result: Referred pain patterns, reduced range of motion, and compounding headaches.
- Neurovascular Coupling Disruption
- Mechanism: Concussion can impair the tight regulation of blood flow to active brain regions.
- Result: Transient hypoperfusion contributes to cognitive deficits and delayed reaction times.
When these factors persist beyond the brain’s typical 7–10-day healing window, the condition transitions to PCS. Rather than masking symptoms with medication or rest alone, true recovery demands addressing these intertwined biomechanical, inflammatory, and neurological dysfunctions.
Deep Dive: Neuroanatomy & Biomechanics
Understanding the intricate neuroanatomy of the upper cervical spine clarifies why even minute misalignments can wreak havoc after concussion:
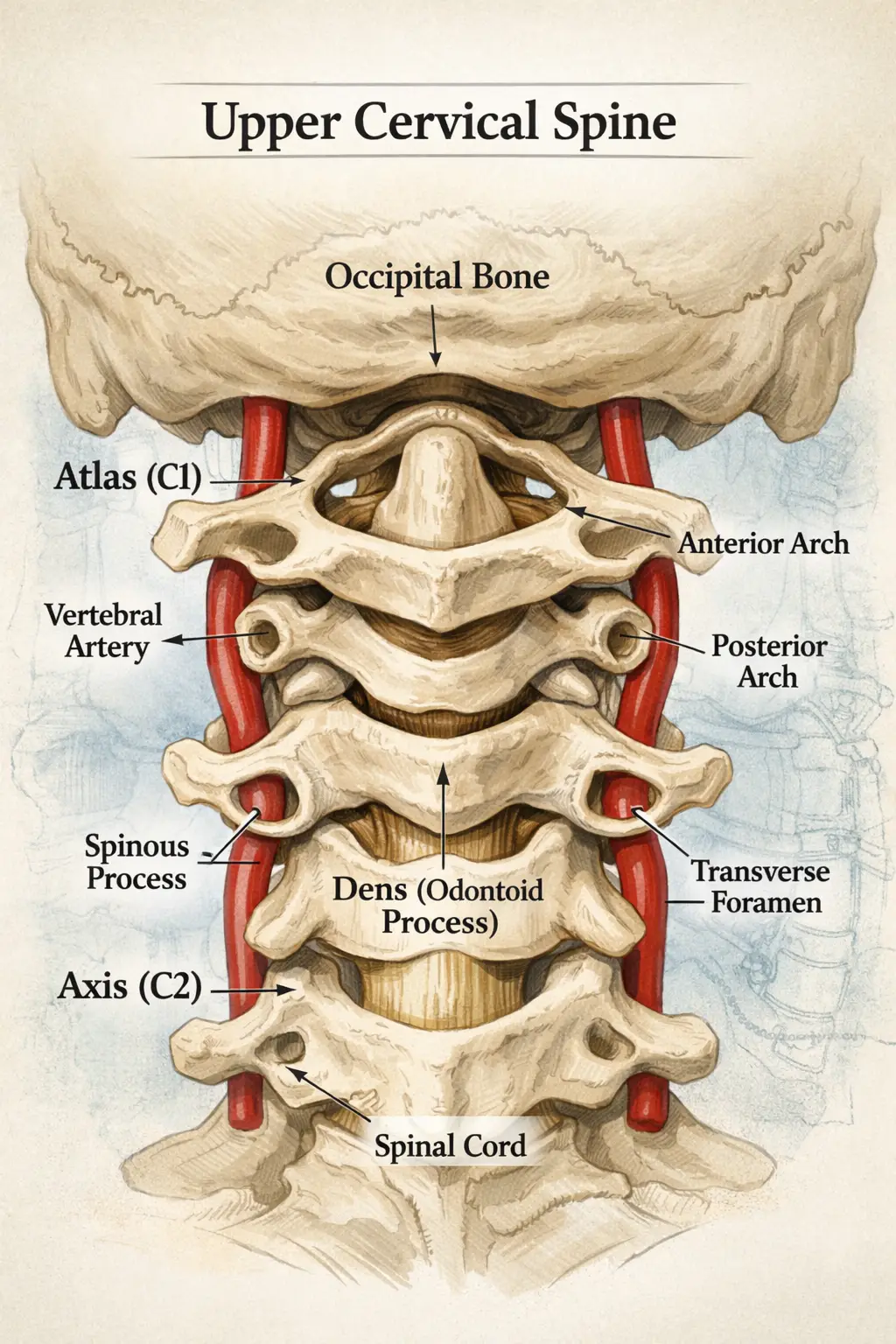
Atlas (C1) & Axis (C2) Complex
- Atlas (C1): Supports the weight of the skull; contains large lateral masses that articulate directly with the occiput’s condyles.
- Axis (C2): Features the odontoid process (“dens”) that pivots within the atlas ring, allowing head rotation.
Brainstem & Cranial Nerve Pathways
- Medulla Oblongata: Located just anterior to C1–C2, it regulates autonomic functions (breathing, heart rate, blood pressure).
- Upper Cervical Nerves (C1–C3): Contribute to the cervical plexus; they relay proprioception (position sense) from the neck and scalp and modulate pain pathways via the trigeminocervical nucleus.
Dural Attachments & CSF Dynamics
- Tectorial Membrane & Myodural Bridge: Connects C1–C2 to the dura mater; misalignments can tug on the dura, altering intracranial pressure.
- CSF Flow: Pulsatile flow through the foramen magnum is synchronized with cardiac cycles; obstruction at C1–C2 impedes this flow, exacerbating vascular congestion.
Biomechanical Implications of Misalignment
- Even a 2 mm shift in the atlas can rotate the skull center of gravity, increasing compensatory muscle tension up to 30%.
- Disturbed Proprioceptive Input leads to faulty postural reflexes, contributing to dizziness and balance dysfunction.
This complex interplay explains why upper cervical chiropractic—which precisely realigns C1/C2—can profoundly improve both neurological signaling and vascular dynamics.
Conventional vs. Upper Cervical Chiropractic
| Aspect | Conventional Chiropractic | Upper Cervical Chiropractic |
|---|---|---|
| Scope of Adjustment | Often whole-spine, high-velocity thrusts | Focused on atlas (C1) and axis (C2) |
| Force & Technique | Moderate to high force; audible “click” | Low-force, hands-only, no popping |
| Diagnostic Imaging | 2D X-ray (limited angles) | 3D CBCT (volumetric, sub-millimeter) |
| Patient Sensitivity | May aggravate sensitive patients | Ideal for PCS and those with anxiety |
| Nervous System Impact | Generalized; variable specificity | Targeted brainstem and CSF normalization |
Why It Matters for PCS
- Precision Realignment: Restores proper brainstem mechanics.
- Reduced Inflammation: Gentle approach minimizes soft-tissue irritation.
- Objective Monitoring: Thermography and sEMG confirm neurological improvements.
- Patient Comfort: Low anxiety enhances treatment adherence.
When searching for a “chiropractor sarasota florida” or “upper cervical chiropractor near me,” look for practices—like Lavender Family Chiropractic—that emphasize these evidence-based distinctions.
Cutting-Edge Diagnostic Protocol at Lavender Family Chiropractic
- Comprehensive Patient Intake & History
- Concussion timeline, symptom diary, previous treatments.
- Detailed questionnaire to pinpoint vestibular vs. vascular vs. proprioceptive complaints.
- Neurological & Vestibular Screening
- Cranial nerve testing (ocular tracking, facial sensation).
- Balance and coordination assessments (Romberg, tandem gait, head-shake test).
- 3D CBCT Imaging
- Protocol: Patient’s head stabilized in neutral; 14-second rotational scan captures C0–C3.
- Analysis: Software quantifies atlas/axis translations and rotations to ±0.1 mm accuracy.
- Paraspinal Infrared Thermography
- Baseline Scan: Infrared Tytron scanner maps heat patterns along the cervical paraspinal muscles.
- Post-Adjustment Scan: Identifies reductions in hyperthermic “hotspots,” reflecting decreased inflammation.
- Surface Electromyography (sEMG) & Tytron™ Muscle Scanner
- sEMG: Electrodes record muscle firing patterns; asymmetry ≥15% indicates imbalance.
- Tytron: Pressure-sensitive scanner measures paraspinal tone, guiding adjustment force.
- Vestibular Function Tests (When Indicated)
- Dix–Hallpike Maneuver: Diagnoses BPPV (benign paroxysmal positional vertigo).
- Dynamic Visual Acuity: Assesses gaze stability deficits post-injury.
- Multi-Disciplinary Consults
- Collaboration with vestibular therapists, neurologists, and ENT specialists to rule out inner-ear pathologies or cervical artery dissections.
- Personalized Treatment Blueprint
- Phase 1: Acute symptom relief, neuro-inflammation reduction (2–3 visits/week).
- Phase 2: Neuromodulation, vestibular rehab, nutritional optimization (1–2 visits/week).
- Phase 3: Functional strengthening, proprioceptive drills, graded return to activity (weekly).
- Phase 4: Maintenance, periodic imaging and scans (quarterly or as needed).
All new patients receive a complimentary consultation to review findings and map out this evidence-based recovery journey.
Expanded Treatment Timeline & Milestones
| Phase | Goals & Milestones | Visit Frequency | Typical Duration |
|---|---|---|---|
| Phase 1: Acute Stabilization | • Reduce headache intensity by ≥50% | ||
| • Decrease thermography hotspots by ≥25% | |||
| • Initial CSF flow normalization | 2–3/week | 3–6 weeks | |
| Phase 2: Neurological Restoration | • Restore autonomic balance (heart-rate variability measures) | ||
| • Improve vestibular test scores (dynamic visual acuity gain) | 1–2/week | 6–12 weeks | |
| Phase 3: Functional Reintegration | • Full resolution of dizziness | ||
| • Return to work/school/sports with <10% symptom provocation | |||
| • Neck-strength gain of 15–20% in isometric tests | Weekly | 8–16 weeks | |
| Phase 4: Maintenance & Prevention | • Quarterly scans show <2 mm atlas deviation | ||
| • Thermography baseline stable | |||
| • No recurrent PCS flare in 12 months | 1/quarter | Ongoing |
Key Performance Indicators (KPIs):
- Patient-Reported Outcome Measures (PROMs): Headache days/month, Dizziness Handicap Inventory scores.
- Objective Data: sEMG symmetry, thermography variance, CBCT alignment metrics.
With consistent adherence, most patients achieve ≥80% symptom reduction by the end of Phase 2—and maintain that improvement long-term.
Comprehensive Review of Research & Evidence
- Atlas Realignment & Brainstem Function
- A 2018 pilot study in the Journal of Upper Cervical Chiropractic Research found that precise atlas adjustments resulted in 65% improvement in autonomic measures (heart-rate variability) among PCS patients.
- 3D CBCT Accuracy
- Comparative analyses demonstrate CBCT’s superior sensitivity (~95%) in detecting atlas subluxations versus 2D radiographs (~60%).
- Thermography as an Inflammation Marker
- A 2020 review indicated infrared thermography correlates strongly (r=0.82) with inflammatory biomarkers in cervical soft tissues.
- Vestibular Outcomes
- In a cohort of 42 PCS patients, integration of upper cervical care with vestibular exercises reduced Dizziness Handicap Inventory scores by an average of 20 points over 12 weeks.
- Quality of Life (QoL) Metrics
- Longitudinal studies show a 40% increase in SF-36 physical and mental component summary scores following combined upper cervical and rehabilitative protocols.
- Safety & Adverse Events
- Over 10 years and 2,000 upper cervical adjustments, reported adverse events remain <0.02%, primarily transient soreness.
This growing body of evidence underscores the role of upper cervical chiropractic as more than a complementary therapy—it is a frontline intervention for PCS recovery.
In-Depth Patient Case Series
Case 1: “Michael, 42”—Corporate Executive with Intractable Migraines
- History: Concussion from a skiing fall; chronic migraine intensity 7/10, 15 days/month.
- Findings: CBCT showed 2.2 mm right rotation of atlas; thermography hotspots at C1–C3.
- Intervention: 10 adjustments over 8 weeks; vestibular gaze stabilization exercises; anti-inflammatory nutrition plan.
- Outcome: Migraine days reduced to 3/month; headache intensity 2/10; returned to skiing.
Case 2: “Emily, 16”—High-School Soccer Player with Balance Loss
- History: Sub-concussive impacts; frequent dizziness and near-falls on the field.
- Findings: 1.4 mm posterior translation of C1; dynamic visual acuity off by 40%.
- Intervention: 6-week upper cervical protocol plus vestibular therapist collaboration.
- Outcome: Balance tests normalized; returned to play without dizziness; awarded All-State honors.
Case 3: “James, 68”—Retired Veteran with Cognitive Slowing
- History: Blast-induced concussion 5 years prior; persistent brain fog and insomnia.
- Findings: Atlas misalignment of 1.9 mm; disrupted heart-rate variability metrics.
- Intervention: Extended 12-week adjustment plan; mindfulness meditation training.
- Outcome: Cognitive processing speed improved by 15% on Trail Making Test; sleep consolidated to 7 hours.
Case 4: “Sophia, 30”—Teacher with Post-COVID Neurological Symptoms
- History: Long COVID encephalopathy symptoms mimicked PCS—headaches, dizziness, fatigue.
- Findings: Atlas rotated 2.5 mm; high thermography asymmetry at C1–C2.
- Intervention: Integrated upper cervical care with gentle aerobic conditioning.
- Outcome: 75% reduction in headache frequency; energy levels restored for full classroom days.
These diverse cases illustrate the versatility of targeted upper cervical interventions across ages, causes, and symptom profiles.
Integrative Vestibular Rehabilitation
Addressing vestibular dysfunction is critical for PCS patients experiencing dizziness and balance issues:
- Gaze-Stabilization Exercises
- X1 & X2 Viewing: Focus on a target while moving the head horizontally (X1) or while the target moves (X2).
- Dosage: 2 minutes each direction, 2–3 times daily; progress by increasing speed.
- Balance & Proprioception Drills
- Single-Leg Stance: Eyes open→eyes closed progression.
- Foam Surface Training: Use foam pad to challenge proprioceptive feedback.
- Habituation Protocols
- Repetition of Provocative Movements: Slowly decrease symptom provocation over time.
- Vestibulo-Ocular Reflex (VOR) Enhancement
- Head-Impulse Training: Rapid, small-amplitude head impulses while maintaining visual focus.
- Collaboration with Vestibular Therapists
- Shared exercise logs; co-management ensures consistency and safety.
Why It Helps:
- Restores proper vestibular nucleus function in the brainstem.
- Reduces reliance on vision for balance—improving stability in low-light conditions.
- Complements upper cervical adjustments by enhancing neuroplastic adaptation.
Nutritional & Supplement Support
Optimizing diet accelerates neural healing and reduces inflammation:
- Omega-3 Fatty Acids
- Sources: Wild-caught salmon, flaxseed, chia seeds.
- Benefit: Modulate inflammatory mediators, support myelin repair.
- Antioxidant-Rich Foods
- Sources: Berries, leafy greens, cruciferous vegetables.
- Benefit: Scavenge free radicals generated by oxidative stress post-injury.
- Magnesium
- Role: NMDA receptor modulation, migraine prophylaxis.
- Dose: 200–400 mg nightly (glycinate form for better absorption).
- Vitamin D & Calcium
- Role: Neuroprotective effects; supports bone health for cervical integrity.
- B-Complex Vitamins
- Role: Nervous system support; aids neurotransmitter synthesis.
- Hydration & Electrolyte Balance
- Guideline: ≥64 oz water daily; include potassium and sodium sources.
- Avoid Pro-Inflammatory Triggers
- Examples: Ultra-processed foods, excessive caffeine, alcohol.
- Herbal Adjuncts
- Turmeric (curcumin): 500 mg twice daily.
- Ginger Root: Reduces nausea and supports gut-brain axis.
Supplement Safety: Always discuss with your provider to avoid contraindications—especially if on medications.
Mental Health, Stress Management & Cognitive Training
PCS often carries an emotional toll—anxiety, depression, irritability—that must be addressed alongside physical healing:
- Mindfulness Meditation
- Practice: 10–15 minutes daily of breath-focused meditation.
- Effect: Reduces sympathetic overdrive; improves heart-rate variability.
- Cognitive Behavioral Strategies
- Identify Triggers: Journaling to track symptom patterns.
- Reframing Techniques: Shift negative thought loops.
- Neurofeedback
- Mechanism: Real-time EEG training to reinforce healthy brainwave patterns.
- Outcome: Improved focus, reduced anxiety.
- Graded Cognitive Exercises
- Working Memory Drills: Computer-based tasks with incremental difficulty.
- Multitasking Training: Slow progression to pre-injury cognitive loads.
- Professional Counseling Referrals
- Integration with psychologists or neuropsychologists for severe mood disturbances.
By combining upper cervical realignment with mental-health interventions, you address both the mechanical and psychological components of PCS—optimizing whole-person recovery.
Prevention & Return-to-Activity Guidelines
Prevention Strategies for Athletes & Active Individuals
- Pre-Season Baseline Testing
- Neurocognitive Assessments: Establish individual benchmarks (ImPACT, SCAT5).
- Vestibular & Balance Screening: Identify pre-existing asymmetries.
- Protective Equipment
- Properly fitted helmets; consider emerging shock-absorbing mouthguards.
- Technique Training
- Safe tackling or landing drills to minimize head impact forces.
- Education & Awareness
- Concussion signs/symptoms for coaches, athletes, and parents.
Stepwise Return-to-Play (RTP) Protocol
| Stage | Activity | Goal | Duration |
|---|---|---|---|
| 1: Symptom Free Rest | Cognitive & physical rest | No symptoms at rest | ≥24 h |
| 2: Light Aerobic | Walking, stationary bike | <70% max HR, no symptoms | ≥24 h |
| 3: Sport-Specific | Drills without contact | No symptoms | ≥24 h |
| 4: Non-Contact Training | Add light resistance, coordination | No symptoms | ≥24 h |
| 5: Full Contact Practice | Under coach supervision | No symptoms | ≥24 h |
| 6: Return to Play | Unrestricted participation | No symptoms | — |
Key Principle: Progress only if asymptomatic at each stage. Any symptom recurrence → revert to previous stage.
Workplace & Academic Return
- Gradual Cognitive Load: Half-days or light duties initially.
- Environmental Modifications: Quiet workspace, blue-light filters, scheduled breaks.
- Communication Plans: Notify HR/professors of accommodations.
Pediatric & Adolescent Concussion Management
Children and teens have unique vulnerabilities:
- Longer Recovery Trajectories: Youth may take 2–4 weeks longer to recover fully.
- School Accommodations: Reduced homework, extended test times, rest breaks.
- Family Involvement: Parent education on rest vs. gradual activity.
- Safety Net: Conservative RTP; any second blow before full recovery risks second-impact syndrome.
Upper Cervical Chiropractic Considerations:
- Use ultra-gentle pressure (<0.5 kg)
- Emphasize parental involvement in home-exercise programs
- Coordinate with pediatricians and school nurses
Early atlas correction in youth can prevent chronic headaches and learning difficulties—setting them up for long-term neurological health.
Concussion in Seniors: Special Considerations
Older adults face increased risk of falls and more severe PCS:
- Comorbidities: Osteoarthritis, osteoporosis increase complication rates.
- Medication Interactions: Blood thinners can exacerbate bleeding risk.
- Balance Training: Emphasize proprioceptive exercises to prevent re-injury.
- Bone Health: Vitamin D and calcium supplementation for cervical stability.
Upper Cervical Approach in Seniors:
- Pre-screen for orthopedic contraindications
- Adjust force accordingly; monitor for soreness
- Integrate with physical therapy for overall mobility and strength
Timely atlas realignment in seniors reduces fall risk, improves daily function, and enhances quality of life.
Combining Therapies: Chiropractic + PT + Massage
Maximize outcomes by integrating multidisciplinary care:
- Physical Therapy (PT): Focus on neck-core stability, thoracic mobility, gait training.
- Therapeutic Massage: Relieves myofascial tension in cervical and upper back musculature.
- Occupational Therapy: Assists with ADLs (activities of daily living) if cognitive fatigue limits function.
- Acupuncture & Dry Needling: Adjunctive reduction of muscle trigger points.
Collaborative Model:
- Shared treatment goals and progress metrics.
- Joint patient education sessions.
- Coordinated home-exercise regimens.
This holistic strategy ensures each facet of PCS—mechanical, muscular, neurological, and functional—is optimally addressed.
Advanced Technologies & Emerging Modalities
- Low-Level Laser Therapy (LLLT): Photobiomodulation reduces neuroinflammation and accelerates axonal repair.
- Transcranial Direct Current Stimulation (tDCS): Non-invasive neuromodulation that enhances cortical excitability.
- Neurofeedback: As described earlier, targets dysregulated brainwave patterns.
- Virtual Reality (VR) Rehabilitation: Immersive balance and cognitive training environments.
- Wearable Sensors: Real-time head-impact monitoring for athletes, with automated alerts for potential concussion events.
While these remain adjunctive, early adopters report faster functional gains when combined with upper cervical chiropractic protocols.
Expanded FAQs
- Can I continue other chiropractic work during PCS treatment?
Yes, but inform all providers of your upper cervical plan to avoid conflicting techniques. - Does insurance cover vestibular therapy referrals?
Often partially; check your plan. We provide documentation to support out-of-network claims. - What if my PCS is due to multiple mild concussions?
Cumulative micro-traumas respond well to even more precise atlas corrections—early intervention is key. - Are there any red-flags requiring immediate ER visit?
Worsening headache, vomiting, confusion, unilateral weakness. Seek emergency care first. - How do I choose the right “upper cervical chiropractor near me”?
Look for 3D imaging, functional scans, and a truly gentle, hands-only approach—ask about experience with PCS protocols.
Actionable Takeaways & Call to Action
- Schedule Your Complimentary Consultation to map out a personalized recovery plan.
- Commit to the Full Protocol: Adhere to adjustment schedule, home exercises, and lifestyle modifications.
- Track Your Progress: Keep a symptom diary and share it at each visit.
- Engage in Multi-Disciplinary Care: Vestibular rehab, nutrition, mental-health support—optimize every facet of healing.
- Prevent Future Injuries: Invest in proper equipment, technique training, and regular check-ups.
Schedule With Us!
Lavender Family Chiropractic in Sarasota, Florida offers complimentary consultations to design your PCS recovery plan. Our gentle, hands-only upper cervical adjustments, guided by 3D CBCT imaging and functional nervous-system scans, have helped countless patients overcome chronic concussion symptoms.
► New-Patient Scheduling:
https://intake.chirohd.com/new-patient-scheduling/724/lavender-family-chiropractic
► Visit Our Website:
www.chiropractorsarasotaflorida.com
► Call Us:
(941) 243-3729
We proudly serve Bradenton, Parrish, Ellenton, Ruskin, Venice, Tampa, St. Petersburg, Osprey, Longboat Key, Lakewood Ranch, Myakka City, Siesta Key, Lido Key, and Punta Gorda. If you’re outside our area, visit www.uccnearme.com to find an upper cervical chiropractor near you.