Why Do I Have Headaches? Headaches are among the most common health complaints worldwide, affecting millions of people across all ages and walks of life. For some, they’re a fleeting inconvenience, but for others, headaches—particularly migraines—can be debilitating, disrupting work, relationships, and overall quality of life. While many factors contribute to headaches, such as stress, dehydration, or dietary triggers, one often-overlooked cause is dysfunction in the upper cervical complex.
This critical region of the spine, comprising the atlas (C1) and axis (C2) vertebrae, plays a significant role in many cases of chronic headaches and migraines. In this comprehensive exploration, we’ll dive deep into why headaches occur, how the upper cervical complex is involved, and what you can do to find lasting relief. Lavender Family Chiropractic is the Best Upper Cervical Chiropractic office in Sarasota, Florida Servicing local and surrounding areas.
Why Do I Have Headaches? Understanding Headaches- A Universal Experience
Headaches are not a single condition but a symptom with a wide range of causes and presentations. The International Headache Society classifies headaches into primary types, like tension headaches, migraines, and cluster headaches, and secondary types, which stem from underlying conditions like infections, trauma, or structural issues. According to the World Health Organization, nearly half of the global adult population experiences at least one headache annually, with migraines alone affecting over 1 billion people.
The impact of headaches extends beyond physical pain. Chronic headaches can lead to missed workdays, reduced productivity, and emotional distress, including anxiety and depression. For migraine sufferers, the burden is even greater, as attacks often include nausea, vomiting, and extreme sensitivity to light and sound, rendering normal activities impossible. Understanding the root cause of your headaches is the first step toward effective management, and for many, the upper cervical complex holds the key.
Types of Headaches
To appreciate the role of the upper cervical complex, it’s helpful to understand the main types of headaches:
- Tension Headaches: These are the most common, characterized by a tight band-like pain around the head. They’re often linked to stress, poor posture, or muscle tension in the neck and shoulders.
- Migraines: These are intense, often one-sided headaches accompanied by symptoms like nausea, vomiting, and sensitivity to light or sound. Migraines can last hours or days and are often triggered by specific factors like hormonal changes, foods, or environmental stimuli.
- Cluster Headaches: Rare but excruciating, these headaches occur in cycles, causing severe pain around one eye or side of the head.
- Cervicogenic Headaches: These originate from the neck, particularly the upper cervical spine, and are often mistaken for tension headaches or migraines due to their similar pain patterns.
While each type has distinct features, the upper cervical complex can play a role in all of them, especially cervicogenic headaches and certain migraines. Let’s explore this region in detail.
The Upper Cervical Complex: Anatomy and Function
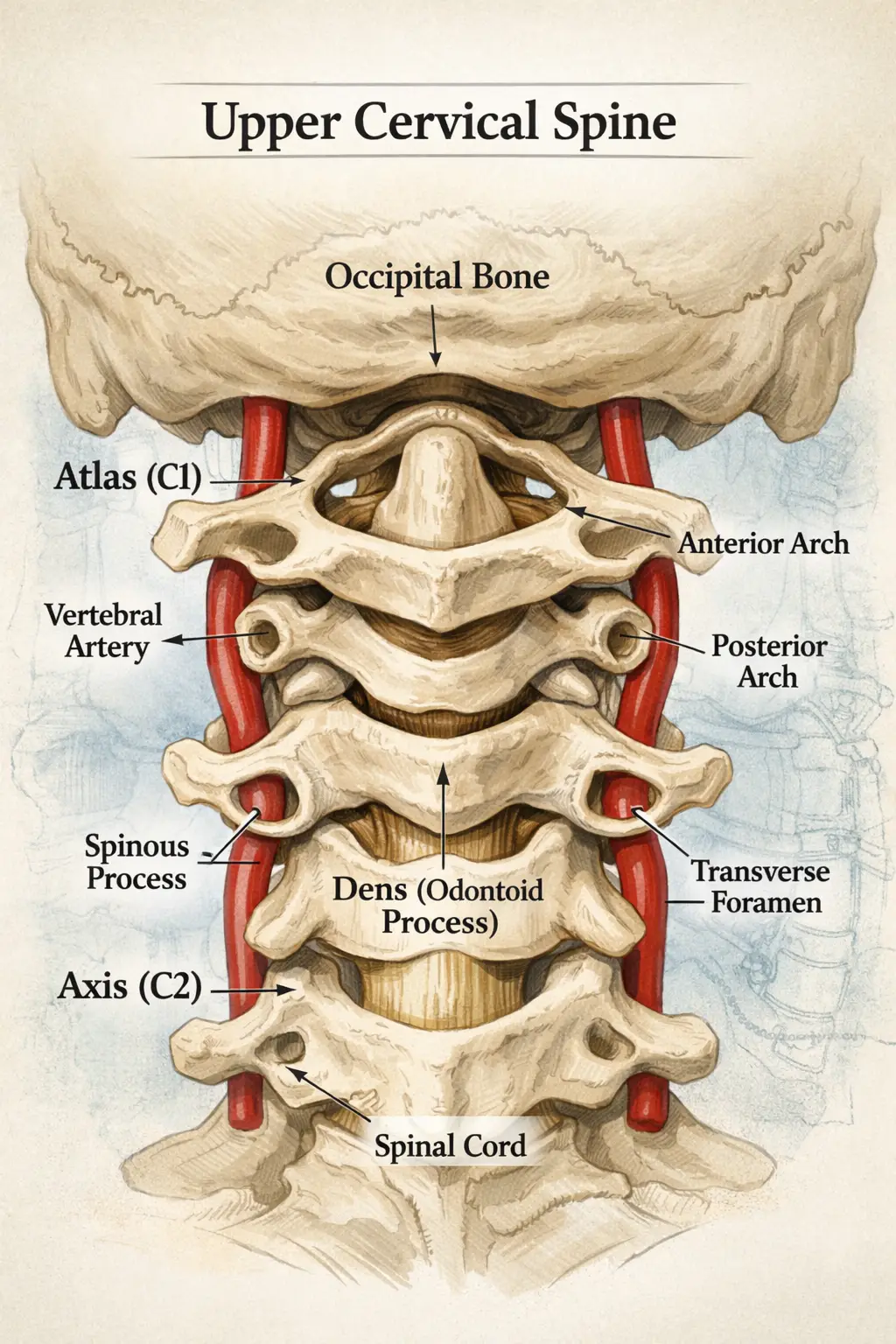
The upper cervical complex refers to the top two vertebrae of the spine: the atlas (C1) and the axis (C2). These vertebrae are unique in both structure and function, making them critical to overall health and a potential source of headaches when dysfunctional.
Anatomy of the Upper Cervical Spine
- Atlas (C1): Named after the mythological figure who carried the world on his shoulders, the atlas is a ring-shaped vertebra that supports the skull. It allows for the nodding motion of the head (e.g., saying “yes”). Unlike other vertebrae, the atlas lacks a central body and has no intervertebral disc, making it highly mobile but less stable.
- Axis (C2): The axis sits directly below the atlas and features a bony projection called the odontoid process (or dens), which acts as a pivot point. This allows the head to rotate side to side (e.g., saying “no”). Together, the atlas and axis enable a wide range of head movements while protecting vital structures.
The upper cervical complex is surrounded by a dense network of ligaments, muscles, and nerves, including the suboccipital muscles, which connect the skull to the spine, and the suboccipital nerves, which transmit sensory information. Additionally, the vertebral arteries, which supply blood to the brain, pass through small openings in the cervical vertebrae, and the brainstem, a critical neurological hub, lies just above the atlas.
Why the Upper Cervical Complex Matters
The upper cervical spine’s role in headaches stems from its unique anatomy and its influence on three key systems:
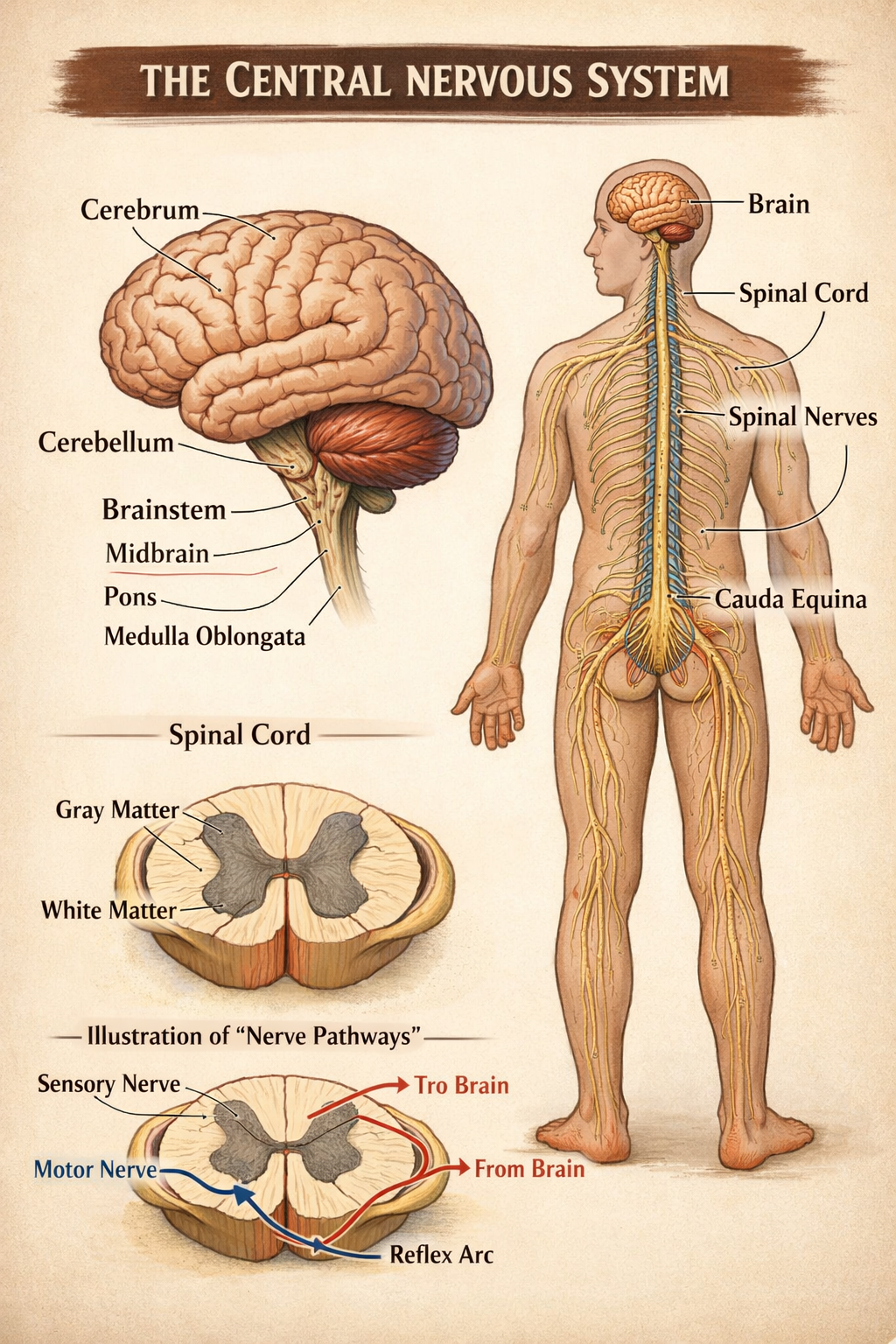
- Neurological System: The brainstem and upper spinal cord, located at the junction of the skull and spine, regulate functions like pain perception, balance, and autonomic processes (e.g., heart rate, breathing). Misalignments in the atlas or axis can irritate nearby nerves or stress the brainstem, amplifying pain signals or triggering headaches.
- Muscular System: The suboccipital muscles and other neck muscles are highly sensitive to changes in spinal alignment. When the upper cervical vertebrae are misaligned, these muscles can become tight or spasmodic, leading to tension that radiates to the head.
- Vascular System: The vertebral arteries supply about 20% of the brain’s blood flow. Any restriction or compression in the upper cervical region can reduce blood flow, contributing to migraines or other vascular headaches.
Given its role as a structural and functional crossroads, even minor issues in the upper cervical complex can have widespread effects, including chronic headaches and migraines.
How the Upper Cervical Complex Contributes to Headaches
When the atlas or axis becomes misaligned—often due to trauma, poor posture, or repetitive strain—it can disrupt the delicate balance of the upper cervical region, leading to headaches through several mechanisms. Below, we’ll explore these mechanisms in detail, along with the science behind them.
1. Nerve Irritation and Compression
The upper cervical spine is rich in sensory nerves, including the greater occipital nerve and lesser occipital nerve, which originate from the C1-C2 region and innervate the scalp and back of the head. Misalignment of the atlas or axis can irritate or compress these nerves, leading to referred pain—pain felt in a different area than its source. This is a hallmark of cervicogenic headaches, which often start at the base of the skull and radiate to the forehead, temples, or behind the eyes.
Additionally, the trigeminal nerve, which is involved in migraine pain, has connections to the upper cervical nerves through a structure called the trigeminocervical nucleus. This nucleus integrates sensory input from the head and neck, meaning that irritation in the upper cervical spine can amplify or trigger migraine-like symptoms. Research published in The Journal of Headache and Pain (2019) supports this, showing that cervical spine dysfunction can lower the threshold for migraine attacks in susceptible individuals.
2. Muscle Tension and Spasms
The suboccipital muscles, located just below the skull, are particularly prone to tension when the upper cervical spine is misaligned. These small but powerful muscles stabilize the head and facilitate fine movements. When the atlas or axis shifts out of alignment, the suboccipital muscles may compensate by tightening or spasming, leading to localized pain and stiffness. This tension can radiate upward, contributing to tension-type headaches or even triggering migraines in those with a predisposition.
Poor posture, such as forward head posture from prolonged computer use or smartphone scrolling, exacerbates this issue. A study in Spine Journal (2020) found that individuals with forward head posture had a higher incidence of tension headaches, likely due to increased strain on the upper cervical muscles and joints.
3. Impaired Blood Flow
The vertebral arteries, which thread through the transverse foramina of the cervical vertebrae, are vulnerable to compression or restriction when the atlas or axis is misaligned. Reduced blood flow to the brain can lead to vascular headaches, including migraines, which are often characterized by throbbing pain and associated symptoms like nausea or visual disturbances. A 2018 study in Cephalalgia highlighted that impaired vertebral artery flow is a potential trigger for migraines, particularly in individuals with cervical spine dysfunction.
Moreover, the upper cervical complex’s proximity to the brainstem means that misalignments can indirectly affect cerebral blood flow regulation. The brainstem houses centers that control vascular tone, and any mechanical stress in this region may disrupt these processes, further contributing to headache development.
4. Brainstem Dysfunction
The brainstem, located just above the atlas, is a critical relay station for pain signals and autonomic functions. Misalignment in the upper cervical spine can place mechanical stress on the brainstem, altering its function. This is particularly relevant for migraines, as the brainstem plays a role in modulating pain perception and processing sensory input. A 2021 review in Frontiers in Neurology suggested that upper cervical dysfunction may contribute to central sensitization—a state where the nervous system becomes hypersensitive to stimuli—making individuals more prone to chronic headaches and migraines.
5. Post-Traumatic Effects
Trauma, such as whiplash from a car accident, a fall, or even repetitive microtraumas from poor ergonomics, can misalign the upper cervical spine. These misalignments may not cause immediate symptoms but can lead to chronic issues over time. For example, a whiplash injury may cause subtle shifts in the atlas or axis, leading to nerve irritation or muscle tension that manifests as headaches months or even years later. A 2017 study in The Journal of Orthopaedic & Sports Physical Therapy found that individuals with a history of whiplash were more likely to develop cervicogenic headaches due to upper cervical dysfunction.
Recognizing Upper Cervical Involvement in Your Headaches
Not all headaches are caused by the upper cervical complex, but certain signs and symptoms suggest this region may be involved. Consider the following:
- Pain Location: Headaches that start at the base of the skull or back of the neck and radiate to the forehead, temples, or behind the eyes are often cervicogenic in origin.
- Neck Symptoms: Stiffness, pain, or reduced range of motion in the neck, especially when turning or tilting the head, may indicate upper cervical involvement.
- Postural Triggers: Headaches that worsen with prolonged sitting, computer work, or looking down at a phone suggest a link to the cervical spine.
- Trauma History: A past injury, such as whiplash, a sports-related concussion, or a fall, increases the likelihood of upper cervical dysfunction.
- Associated Symptoms: Dizziness, jaw pain, or ringing in the ears (tinnitus) alongside headaches may point to the upper cervical complex, as these symptoms can arise from nerve or vascular irritation in this region.
- Treatment Resistance: If medications, stress management, or dietary changes haven’t fully resolved your headaches, the upper cervical spine may be an underlying factor.
Keeping a headache diary can help you identify patterns and triggers. Note the timing, location, intensity, and associated symptoms of your headaches, as well as any activities or positions that worsen or relieve them. This information can guide your healthcare provider in diagnosing the role of the upper cervical complex.
Addressing Upper Cervical Dysfunction for Headache Relief
If the upper cervical complex is contributing to your headaches, targeted interventions can provide significant relief. Below, we’ll explore evidence-based approaches to address this issue, from conservative treatments to lifestyle changes.
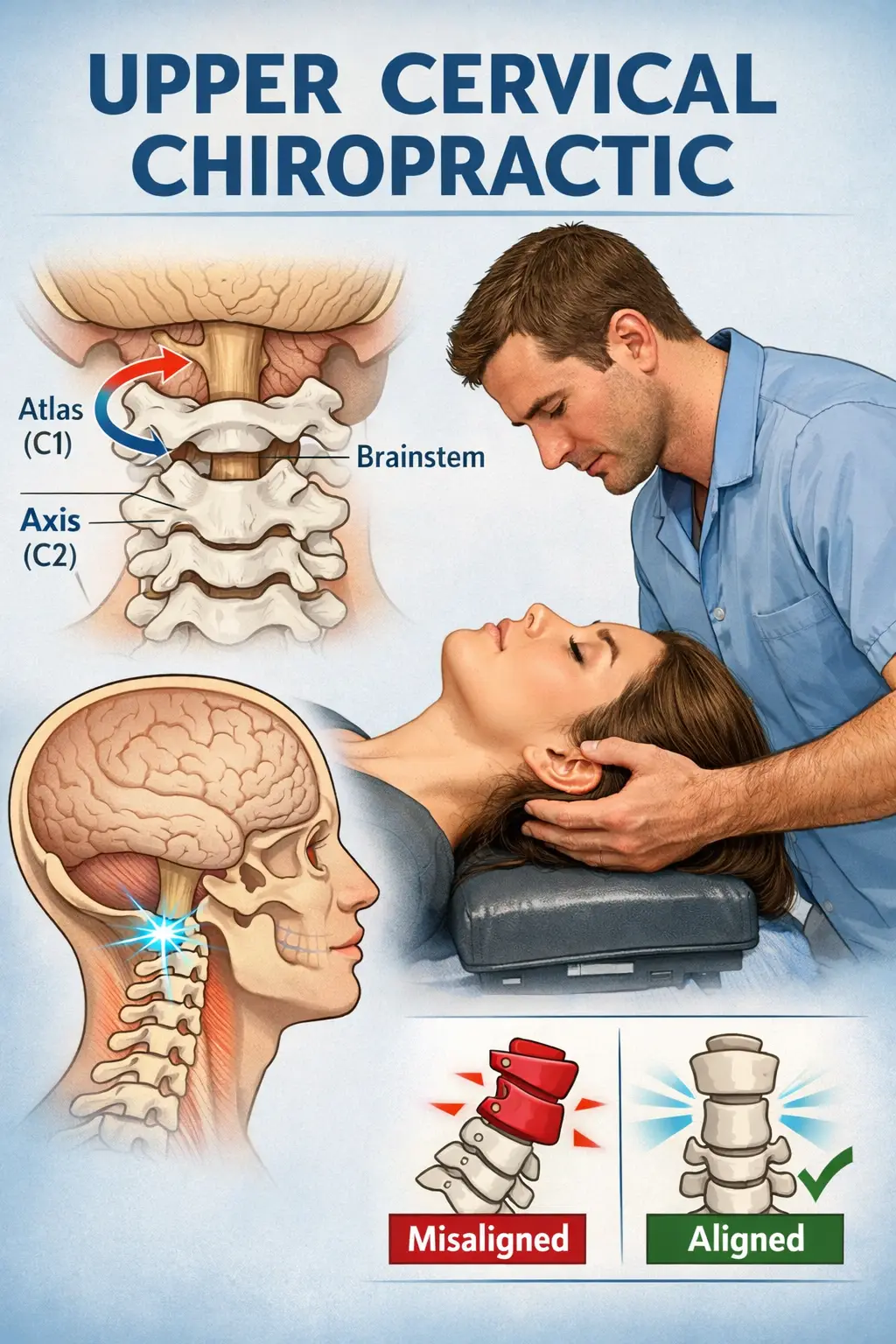
1. Upper Cervical Chiropractic Care
Upper cervical chiropractic techniques, such as , Knee Chest Upper Cervical (AHKC), NUCCA (National Upper Cervical Chiropractic Association) or Atlas Orthogonal, focus on precisely correcting misalignments in the atlas and axis. These methods use gentle, non-invasive adjustments to restore proper alignment, reducing nerve irritation, muscle tension, and vascular restrictions. Unlike traditional chiropractic adjustments, upper cervical techniques avoid high-velocity thrusts, making them suitable for individuals with sensitive necks or a history of trauma.
Cone Beam Computed Tomography (CBCT) imaging is a specialized, three-dimensional radiographic technique that provides detailed visualizations of the craniofacial structures, including the upper cervical complex, with high precision and minimal radiation exposure compared to traditional CT scans. Widely used in dentistry, orthodontics, and upper cervical chiropractic care, CBCT produces high-resolution images of bones, joints, and soft tissues, enabling clinicians to assess misalignments, joint abnormalities, or pathologies that may contribute to headaches or migraines.
Its ability to capture a 360-degree view of the atlas (C1) and axis (C2) vertebrae makes it invaluable for diagnosing subtle misalignments or structural issues in the upper cervical spine that could irritate nerves or impede blood flow. While CBCT is non-invasive and efficient, its use should be guided by clinical necessity to minimize radiation exposure, and it’s often paired with other diagnostic tools for a comprehensive evaluation.
A 2019 study in Chiropractic & Manual Therapies found that upper cervical chiropractic care significantly reduced the frequency and intensity of cervicogenic headaches in patients with confirmed atlas misalignments. Many patients also report improvements in migraines and tension headaches after treatment. When seeking a chiropractor, look for one with specific training in upper cervical techniques, as this area requires specialized expertise.
2. Physical Therapy and Rehabilitation
Physical therapy can address muscle imbalances, improve mobility, and strengthen the neck to support the upper cervical spine. A physical therapist may use techniques like:
- Manual Therapy: Gentle mobilization of the cervical joints to restore alignment and reduce tension.
- Therapeutic Exercises: Strengthening and stretching exercises for the suboccipital muscles, trapezius, and deep neck flexors to improve stability and posture.
- Postural Training: Guidance on maintaining proper head and neck alignment during daily activities.
A 2020 meta-analysis in Physical Therapy showed that manual therapy combined with exercise was effective in reducing the frequency and severity of cervicogenic headaches, with benefits lasting up to six months.
3. Posture Correction and Ergonomics
Poor posture is a leading cause of upper cervical dysfunction, particularly in the digital age. Forward head posture, often caused by prolonged computer use or smartphone scrolling, places significant strain on the atlas and axis. To counteract this:
- Optimize Your Workspace: Ensure your computer monitor is at eye level, your chair supports your lower back, and your keyboard allows your elbows to rest at a 90-degree angle.
- Take Breaks: Stand, stretch, or walk every 30-60 minutes to relieve neck tension.
- Practice Postural Awareness: Keep your head aligned with your spine, avoiding forward tilting or slouching.
Wearable posture correctors or apps that remind you to check your posture can also be helpful. Over time, these changes can reduce strain on the upper cervical complex and decrease headache frequency.
4. Stress Management
Stress is a common headache trigger, often exacerbating muscle tension in the neck. Techniques like mindfulness meditation, deep breathing, or yoga can reduce stress and relax the suboccipital muscles. A 2018 study in The Journal of Headache and Pain found that mindfulness-based stress reduction significantly reduced migraine frequency in patients with cervical spine dysfunction, suggesting a synergistic benefit when combined with physical treatments.
5. Lifestyle Modifications
Several lifestyle factors can support upper cervical health and reduce headaches:
- Hydration: Dehydration can exacerbate headaches, particularly tension-type headaches. Aim for at least 8-10 glasses of water daily, adjusted for your activity level and climate.
- Sleep Hygiene: Poor sleep posture, such as sleeping on your stomach, can strain the upper cervical spine. Use a supportive pillow that keeps your neck aligned with your spine, and aim for 7-9 hours of quality sleep.
- Dietary Considerations: Certain foods, like caffeine, alcohol, or processed foods, can trigger migraines. A balanced diet rich in anti-inflammatory foods (e.g., fruits, vegetables, omega-3 fatty acids) may reduce headache frequency.
- Exercise: Regular physical activity, such as walking, swimming, or yoga, can improve circulation, reduce muscle tension, and support spinal health.
6. Medical Evaluation and Multidisciplinary Care
If your headaches persist despite conservative measures, consult a healthcare provider to rule out other causes, such as:
- Hormonal Imbalances: Conditions like premenstrual syndrome or thyroid dysfunction can trigger headaches.
- Medication Overuse: Overuse of pain relievers can lead to rebound headaches.
- Neurological Conditions: Rare but serious conditions, like tumors or vascular abnormalities, may require imaging (e.g., MRI or CT) for diagnosis.
A multidisciplinary approach, combining upper cervical chiropractic care, physical therapy, and medical management, may be necessary for complex cases. Neurologists, pain specialists, or headache clinics can provide comprehensive evaluations and tailored treatment plans.
Case Studies: Real-Life Examples
To illustrate the impact of the upper cervical complex, consider these hypothetical scenarios based on common clinical presentations:
Case 1: Sarah, 32, Office Worker
Sarah, a 32-year-old office worker, experienced daily tension headaches that started at the base of her skull and radiated to her temples. She attributed them to stress and long hours at her desk. A physical exam revealed forward head posture and restricted movement in her upper cervical spine. After six weeks of upper cervical chiropractic adjustments and postural exercises, Sarah’s headache frequency dropped to once a week, and her neck mobility improved significantly.
Case 2: Michael, 45, Post-Whiplash Migraines
Michael developed migraines after a car accident five years prior. His symptoms included throbbing pain on one side of his head, nausea, and light sensitivity. An upper cervical chiropractor identified an atlas misalignment, likely from the whiplash injury. After three months of targeted adjustments and physical therapy, Michael’s migraines reduced from twice weekly to once monthly, with less severe symptoms.
These cases highlight how addressing upper cervical dysfunction can lead to meaningful improvements, even in chronic headache sufferers.
Preventing Upper Cervical-Related Headaches
Prevention is key to reducing headache frequency and severity. Here are practical steps to maintain upper cervical health:
- Regular Check-Ups: Schedule periodic evaluations with a chiropractor or physical therapist to catch misalignments early.
- Ergonomic Awareness: Invest in ergonomic furniture and accessories, like a standing desk or cervical pillow, to support spinal health.
- Mindful Movement: Incorporate neck stretches and mobility exercises into your daily routine to keep the upper cervical spine flexible.
- Stress Reduction: Practice stress-relieving activities like meditation or progressive muscle relaxation to prevent muscle tension.
- Stay Active: Regular exercise improves circulation and strengthens the muscles that support the cervical spine.
When to Seek Professional Help
If you suspect your headaches are linked to the upper cervical complex, seek care from a qualified professional, such as:
- Upper Cervical Chiropractor: For precise adjustments to the atlas and axis.
- Neurologist: To rule out neurological causes or prescribe medications if needed.
- Physical Therapist: For rehabilitation and posture correction.
- Pain Specialist: For chronic headaches requiring advanced interventions, like nerve blocks.
When choosing a provider, ask about their experience with upper cervical issues and headache management. Be wary of practitioners who promise quick fixes, as lasting relief often requires a combination of treatments and lifestyle changes.
The Science Behind Upper Cervical Care
Research on the upper cervical complex and headaches is growing, with several studies supporting its role:
- A 2020 systematic review in The Journal of Manipulative and Physiological Therapeutics found that upper cervical chiropractic care was effective in reducing cervicogenic headache frequency and intensity, with effects comparable to pharmaceutical treatments but fewer side effects.
- A 2018 study in Headache demonstrated that manual therapy targeting the upper cervical spine improved migraine outcomes in patients with coexisting neck pain.
- A 2021 trial in Pain Medicine showed that correcting atlas misalignments improved blood flow in the vertebral arteries, potentially reducing migraine triggers.
While more research is needed to fully understand the mechanisms, these findings underscore the importance of the upper cervical complex in headache management.
Final Thoughts
Headaches and migraines are complex, with multiple potential causes, but the upper cervical complex is a critical and often overlooked factor. Misalignments in the atlas and axis can irritate nerves, tense muscles, impair blood flow, and stress the brainstem, all of which can trigger or exacerbate headaches. By addressing these issues through targeted interventions like chiropractic care, physical therapy, and lifestyle changes, many individuals find significant relief and improved quality of life.
If you’re struggling with chronic headaches, don’t assume they’re just a part of life. Explore the role of your upper cervical spine with the help of a qualified healthcare provider. Keep a headache diary, prioritize spinal health, and take proactive steps toward lasting relief. Your head—and your overall well-being—will thank you.
Schedule With Us!
Lavender Family Chiropractic in Sarasota Florida offers complimentary consultations to learn more about you. Click the link below!
https://intake.chirohd.com/new-patient-scheduling/724/lavender-family-chiropractic
Visit our Website!
To learn more about us go to http://www.chiropractorsarasotaflorida.com
We also service Bradenton, Parrish, Ellenton, Ruskin, Venice, Tampa, St. Pete, Osprey, Longboat, Lakewood Ranch, Myakka City.
If you are not local, visit www.uccnearme.com to find a doctor in your area!.
Call Us
Our Office number is