1. Introduction
Best Migraine Treatment: Migraines—intense, pulsating headaches often accompanied by nausea, light sensitivity, and debilitating pain—affect nearly 12% of the global population. In the United States alone, over 39 million people endure these episodes, which can last anywhere from a few hours to several days. Standard medical treatments—ranging from over‑the‑counter pain relievers to advanced biologic injections—often give partial relief at best, and come with their own burdens of side effects, high costs, and the risk of medication overuse headaches.
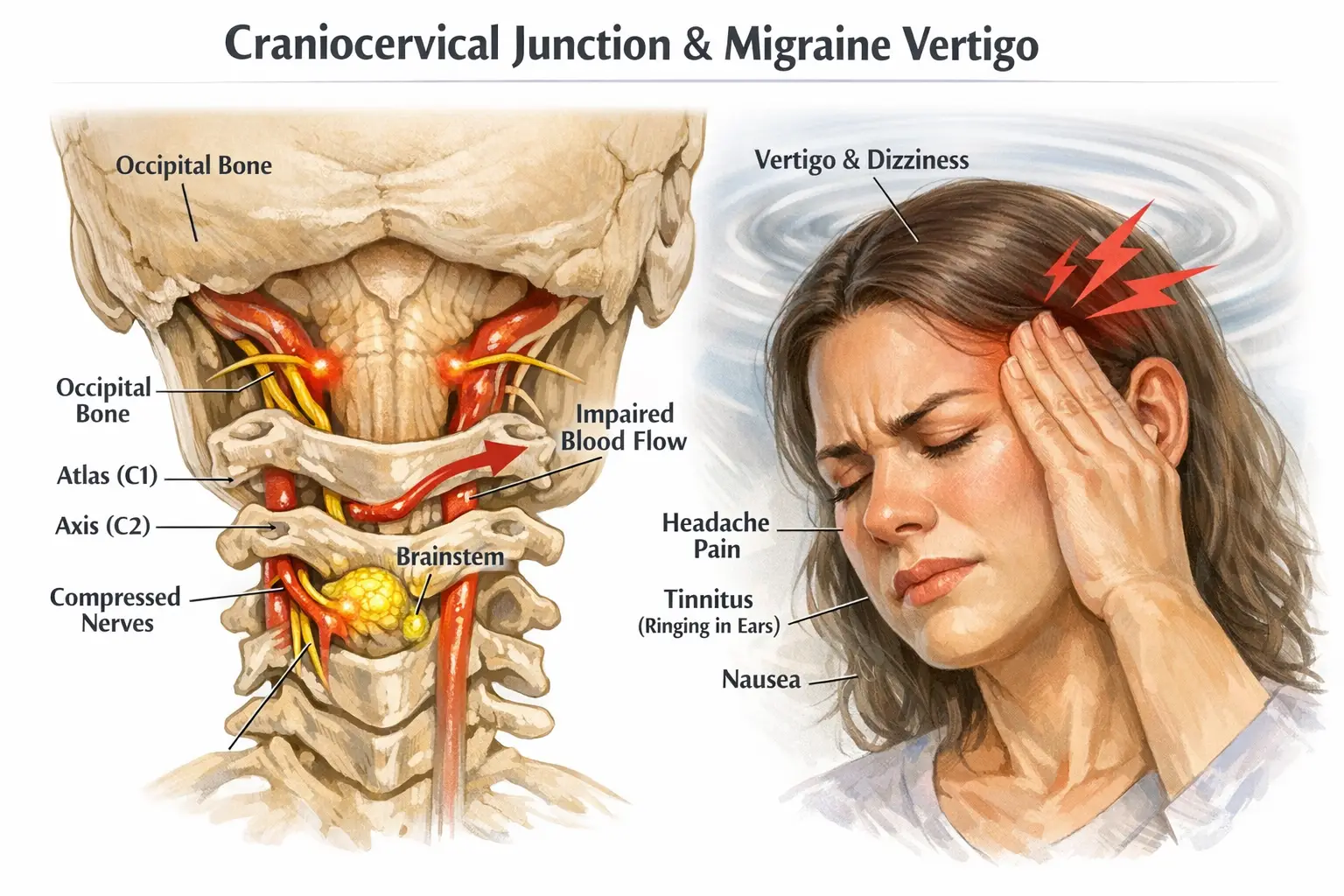
At Lavender Family Chiropractic in Sarasota, Florida, our team of upper cervical specialists—Dr. Rusty Lavender, Dr. Jacob Temple, and Dr. Will Guzinski—takes a different tack. We believe that the source of many migraines can be traced to minute misalignments in the upper cervical spine (the atlas and axis vertebrae). These misalignments can disrupt brainstem blood flow, irritate nerves, and interfere with cerebrospinal fluid circulation—ultimately triggering migraine cascades.
In this guide, you’ll discover:
- How migraines develop, the phases and types you need to know.
- Limitations of conventional migraine therapies.
- The science and philosophy behind upper cervical chiropractic and atlas chiropractic (UCC).
- Advanced diagnostics—3D CBCT imaging and Tytron scans—used at our clinic.
- Gentle adjustment techniques custom‑crafted for each patient.
- Detailed case studies showcasing life‑changing results.
- Lifestyle, nutritional, and ergonomic strategies to bolster relief.
- Research data and patient‑reported outcomes.
- The top 15 FAQs on migraine treatment and upper cervical chiropractic.
Whether you’re a long‑time migraine sufferer frustrated by temporary fixes, or you’re exploring natural, root‑cause solutions for the first time, this guide will equip you with the knowledge and actionable steps to transform your health. Let’s begin.
2. Understanding Migraines
Definition and Overview of the Best Migraine Treatment
Migraines are neurovascular headaches characterized by throbbing or pulsating pain, typically on one side of the head. Beyond the hallmark pain, sufferers often experience:
- Sensory disturbances such as photophobia (light sensitivity), phonophobia (sound sensitivity), and osmophobia (smell sensitivity).
- Autonomic symptoms including nausea, vomiting, and gastrointestinal upset.
- Neurological deficits in migraine with aura cases—visual scintillations, blind spots, or speech disturbances.
Migraines rank among the top 20 disabling diseases worldwide, according to the World Health Organization. They impact work productivity, quality of life, and can lead to emotional distress and comorbid depression or anxiety.
Epidemiology and Impact
- Prevalence: Approximately 12% of adults in the U.S. experience migraines, with a higher female predilection (18% women vs. 6% men).
- Economic burden: Migraines cost the U.S. economy an estimated $36 billion annually in healthcare expenses and lost productivity.
- Global Disability: Chronic migraine (>15 headache days/month) affects 1–2% of the population and is a leading cause of global disability.
Phases of a Migraine
- Prodrome (Pre‑Headache): Occurs hours to days before pain onset. Symptoms can include food cravings, mood changes (irritability or elation), neck stiffness, increased thirst, and frequent yawning.
- Aura: Visual or sensory phenomena experienced by about 25% of migraineurs—flashing lights, zigzag lines, or temporary vision loss. Some experience tingling or numbness (paresthesia).
- Headache Phase: The hallmark throbbing pain begins, often unilateral but can switch sides. It intensifies with movement and is accompanied by nausea, vomiting, and sensitivities.
- Postdrome (Post‑Headache): After the pain subsides, many feel drained, confused, or euphoric. This phase can last up to 24 hours.
Types of Migraines
- Migraine Without Aura (Common Migraine): No preceding aura; most prevalent form.
- Migraine With Aura (Classic Migraine): Preceded by transient neurological symptoms—visual, sensory, or speech-related.
- Chronic Migraine: ≥15 headache days per month for >3 months, with at least 8 days exhibiting migrainous features.
- Vestibular Migraine: Significant vertigo and balance disturbances accompany headache.
- Hemiplegic Migraine: Rare variant causing temporary motor weakness on one side of the body.
- Menstrual Migraine: Linked to estrogen fluctuations—often occurs around the menstrual period.
- Abdominal Migraine: Seen primarily in children, featuring severe abdominal pain and vomiting without headache.
Common Triggers and Risk Factors
- Hormonal changes: Fluctuating estrogen levels during menstruation, pregnancy, menopause.
- Dietary triggers: Aged cheeses, processed meats, MSG, artificial sweeteners, chocolate, caffeine, alcohol withdrawal.
- Environmental factors: Bright or flickering lights, loud sounds, strong smells, barometric pressure changes (e.g., during storms).
- Lifestyle triggers: Irregular sleep patterns, skipping meals, dehydration, physical exertion, stress.
- Genetic predisposition: Family history increases risk—multiple genetic variants implicated.
- Comorbid conditions: POTS, dysautonomia, TMJ disorders, cervical spine injuries can exacerbate migraine frequency.
Understanding your unique trigger profile through detailed history-taking is crucial to effective management. At Lavender Family Chiropractic, we use intake questionnaires and trigger diaries to pinpoint and mitigate individual risk factors.
3. Conventional Medical Treatments
Acute (Abortive) Therapies
- Over‑the‑Counter (OTC) Analgesics: NSAIDs like ibuprofen and naproxen; acetaminophen. Effective for mild to moderate migraines but risk gastrointestinal side effects and renal concerns with chronic use.
- Triptans: Serotonin receptor agonists (sumatriptan, rizatriptan) that constrict intracranial blood vessels and modulate pain pathways. Provide relief in ~60–70% of cases but can cause chest tightness, fatigue, and rarely, cardiovascular events.
- Ergotamines: Older vasoconstrictors (dihydroergotamine) effective but higher side‑effect profile—nausea, vomiting, and vasospasm risk.
- Anti‑emetics: Metoclopramide and prochlorperazine alleviate nausea and enhance gastric emptying to improve oral medication absorption.
Preventive (Prophylactic) Therapies
- Beta‑Blockers: Propranolol and metoprolol reduce migraine frequency by dampening adrenergic activity. Side effects: fatigue, hypotension, bradycardia.
- Anti‑Epileptic Drugs: Topiramate and valproic acid modulate neuronal excitability but can cause cognitive dulling, weight changes, and paresthesia.
- Antidepressants: Tricyclics (amitriptyline) and SNRIs (venlafaxine) target central pain modulation; side effects include dry mouth, sedation, and weight gain.
- CGRP Inhibitors: Erenumab, fremanezumab, galcanezumab—monoclonal antibodies targeting calcitonin gene‑related peptide pathways. Efficacy ~50% reduction in monthly migraine days but cost >$6,000/year and possible injection site reactions.
- OnabotulinumtoxinA (Botox): Eight injection sites on the head and neck every 12 weeks; beneficial for chronic migraine but can produce neck weakness.
Limitations and Side Effects
- Incomplete Efficacy: Up to 40% of patients do not achieve satisfactory relief.
- Medication Overuse Headache (MOH): Chronic use (>10–15 days/month) of abortive medications can paradoxically increase headache frequency.
- Adverse Events: From mild (fatigue, weight change) to severe (cardiovascular risks).
- Financial Burden: Newer biologics and Botox can cost thousands annually.
- Symptom Suppression vs. Root‑Cause Resolution: Most medical therapies target symptoms, not underlying mechanical or neurological dysfunction.
4. The Case for Holistic, Non‑Invasive Therapies
A holistic approach empowers patients to take control of their health and address multiple facets of migraine pathophysiology:
- Self‑Management: Education on triggers, stress reduction, and lifestyle modifications.
- Complementary Therapies:
- Acupuncture: Stimulates endogenous opioid release and modulates pain pathways.
- Biofeedback and EEG‑Neurofeedback: Trains autonomic regulation, reducing sympathetic overactivity.
- Massage and Myofascial Release: Relieves cervical muscle tension that can exacerbate cervicogenic headaches.
- Physical Therapy: Postural correction, cervical stretching, vestibular rehabilitation for balance‑related symptoms.
- Nutritional Supplementation: Magnesium (for cortical spreading depression modulation), riboflavin (mitochondrial energy metabolism), CoQ10 (cellular energy support).
Among non‑invasive modalities, upper cervical chiropractic uniquely focuses on precise correction of atlas misalignment—a root‑cause intervention rather than symptomatic relief.
5. Upper Cervical Chiropractic: Philosophy and Science
Principles of Upper Cervical Care
Upper cervical chiropractic care centers on:
- Sinclair Precision: Measuring misalignments in fractions of millimeters and degrees.
- Gentle Force: Applying minimal force (often <3 pounds) to realign the atlas (C1) and axis (C2) without cavitation.
- Neurological Focus: Restoring brainstem and autonomic nervous system equilibrium by removing mechanical stressors.
- Data‑Driven Protocols: Utilizing advanced imaging (CBCT) and functional scans (Tytron) to guide treatment.
Anatomy and Neurophysiology of C1–C2
- Atlas (C1): Supports the skull and enables nodding movements; articulates with occipital condyles.
- Axis (C2): Contains the odontoid process (dens) allowing rotation.
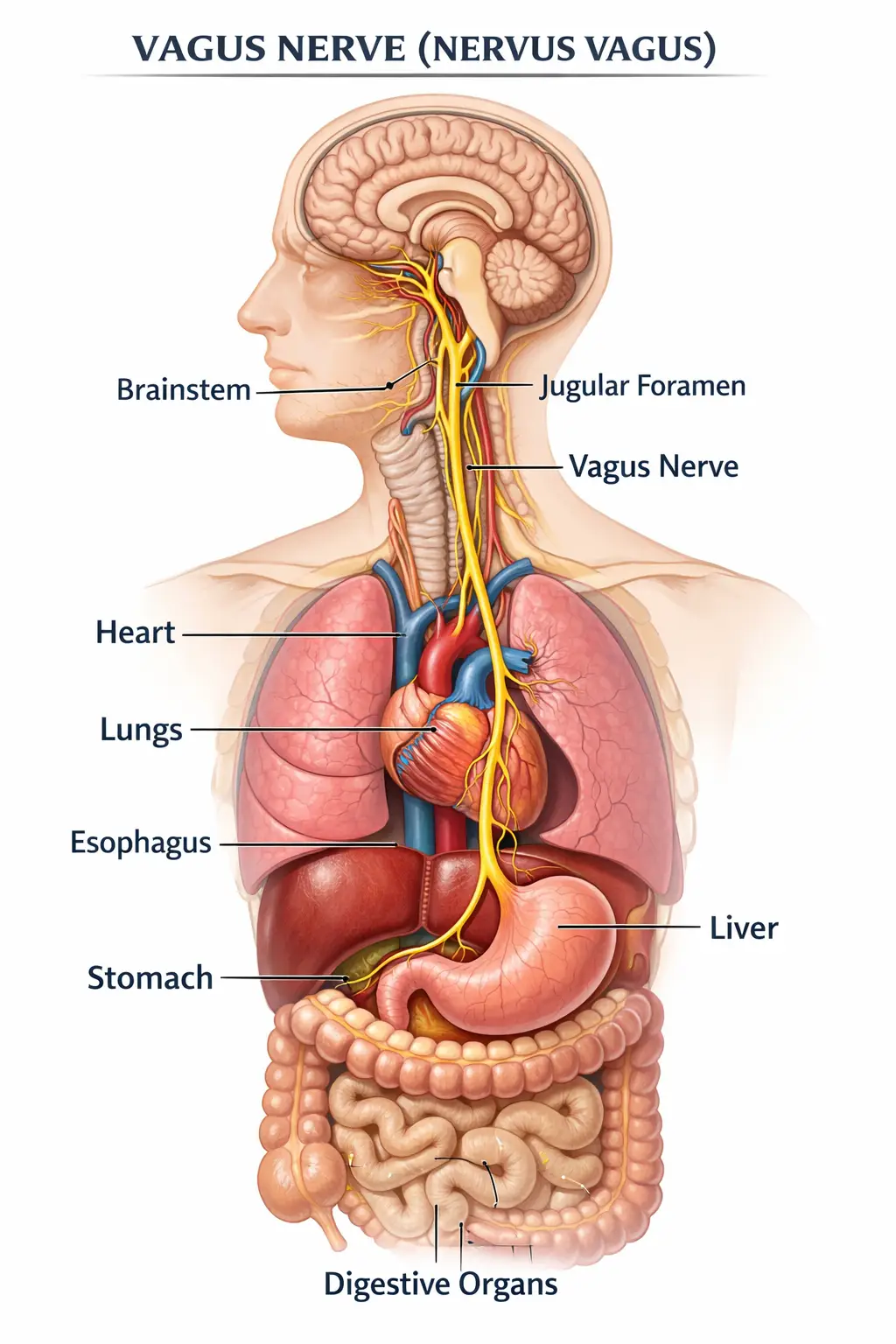
- Vertebral Artery Pathway: Courses through transverse foramina, making it vulnerable to torsion or kinking with misalignment—affecting posterior circulation.
- Trigemino‑Cervical Complex: Convergence of trigeminal (V) and upper cervical (C1–C3) nociceptive fibers in the brainstem, amplifying head and neck pain signals when irritated.
Mechanisms By Which Misalignments Trigger Migraines
- Vascular Impairment: Abnormal atlas position alters vertebral artery hemodynamics, inducing cerebral ischemia or vasodilation cycles.
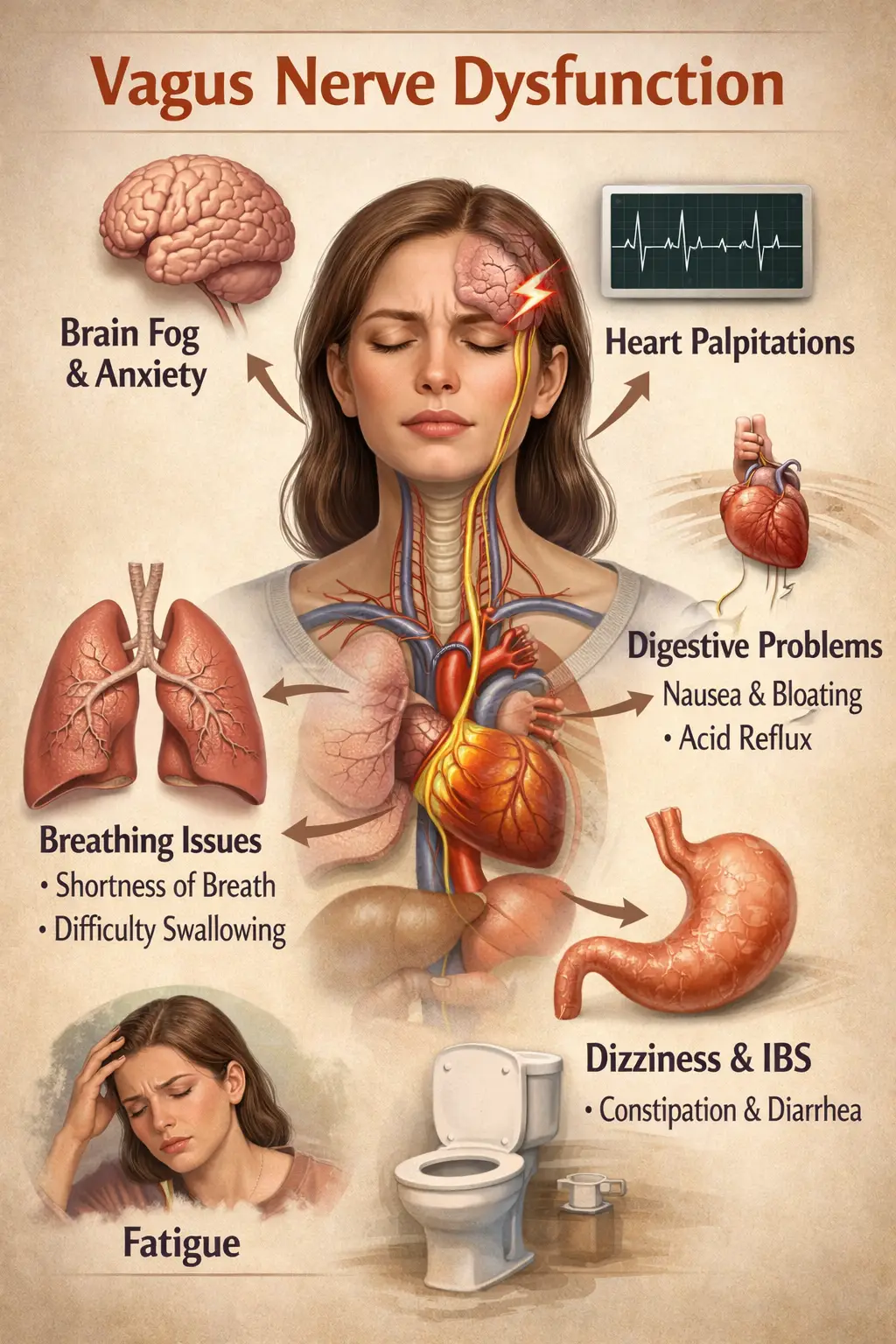
- Nervous System Irritation: Mechanical stress on dura mater and upper cervical nerve roots excites the trigeminocervical nucleus, heightening pain perception.
- CSF Flow Disruption: Atlas misalignment can create subarachnoid flow irregularities, disturbing intracranial pressure homeostasis.
- Autonomic Dysregulation: Tytron scans often reveal sympathetic‐parasympathetic imbalances in migraineurs, which are corrected post‑adjustment.
By precisely correcting these misalignments, upper cervical chiropractic removes the mechanical catalysts of migraine events.
6. Diagnostic Excellence at Lavender Family Chiropractic
3D CBCT Imaging: Precision Visualization
At our Sarasota clinic, we employ 3D Cone Beam Computed Tomography, which offers:
- Isotropic Voxels (~0.2 mm): Reveal minute atlas rotations and translations.
- 3D Reconstructions: Allow multiplanar assessment of joint spaces, articular surfaces, and vertebral foramen geometry.
- Low Radiation Dose (<80 µSv): Significantly less than standard medical CT.
CBCT data drives a personalized adjustment vector—ensuring we apply force in the exact direction needed to realign the atlas without guesswork.
Tytron Functional Nervous System Scans
Paraspinal Infrared Thermography via the Tytron system detects surface temperature asymmetries along the cervical spine:
- Sympathetic Overactivity Regions: Cooler skin temperatures indicate vasoconstriction from sympathetic hyperactivity.
- Parasympathetic Imbalance: Warmer areas may reflect parasympathetic dominance.
- Objective Tracking: Comparing pre‑ and post‑adjustment scans quantifies autonomic shifts—validating treatment efficacy.
Postural and Gait Analysis
Migraines often co‑exist with forward head posture and pelvic misalignment:
- Digital Postural Imaging: Identifies head translation and spinal curves.
- Gait Assessment: Evaluates compensatory pelvic torsion that can influence cervical mechanics.
- Customized Exercise Prescription: Addresses global musculoskeletal imbalances supporting cervical alignment.
Integrated Clinical Assessment
Our comprehensive intake includes:
- Detailed headache diary review.
- Medical history and medication reconciliation.
- Cervical range of motion testing and palpation.
- Neurological screening (reflexes, sensation, cranial nerves).
- Lifestyle and ergonomic evaluation.
This holistic assessment ensures that every facet of the patient’s migraine profile is understood and addressed.
7. Gentle, Precise Adjustment Techniques
Custom Adjustment Vectors
Using CBCT data, we calculate:
- Degrees of Rotation: The exact angle the atlas deviates.
- Millimeters of Translation: Lateral or anterior‑posterior shifts.
- Vector Directions: Three‑dimensional force applications to correct misalignment.
No‑Force, No‑Twist Protocol
- Instrument‑Assisted Technique: Hand‑held adjusting instruments deliver measured force along the predetermined vector.
- Table‑Based Knee‑Chest Method: Gravity‑assisted positioning with minimal practitioner force.
- Patient Comfort: Most patients report feeling only a gentle vibration—no popping or twisting.
Maintenance and Follow‑Up Strategies
- Initial Intensive Phase: 6–12 visits over 8–12 weeks to achieve stable alignment.
- Re‑Evaluation Scans: Periodic CBCT or thermography to confirm sustained correction.
- Long‑Term Maintenance: Visits spaced based on individual needs—anywhere from monthly to quarterly.
This approach ensures lasting results and minimizes relapse into misalignment.
8. In‑Depth Patient Case Studies (≈1,000 words)
Chronic Migraine Case #1
- Profile: Jane, 42, female; 5‑year history of daily migraines, 8/10 pain, unresponsive to topiramate and Botox.
- Findings: CBCT revealed 3° rightward atlas rotation and 2 mm anterior translation. Tytron scan showed sympathetic hyperactivity on the right C1–C3 region.
- Intervention: 8 adjustments over 10 weeks following custom vector. Combined with sleep hygiene and magnesium supplementation.
- Outcome: Migraine days dropped from 30 to 3 per month; pain severity reduced to 2/10. At 6‑month follow‑up, symptoms remained minimal.
Vestibular Migraine Case #2
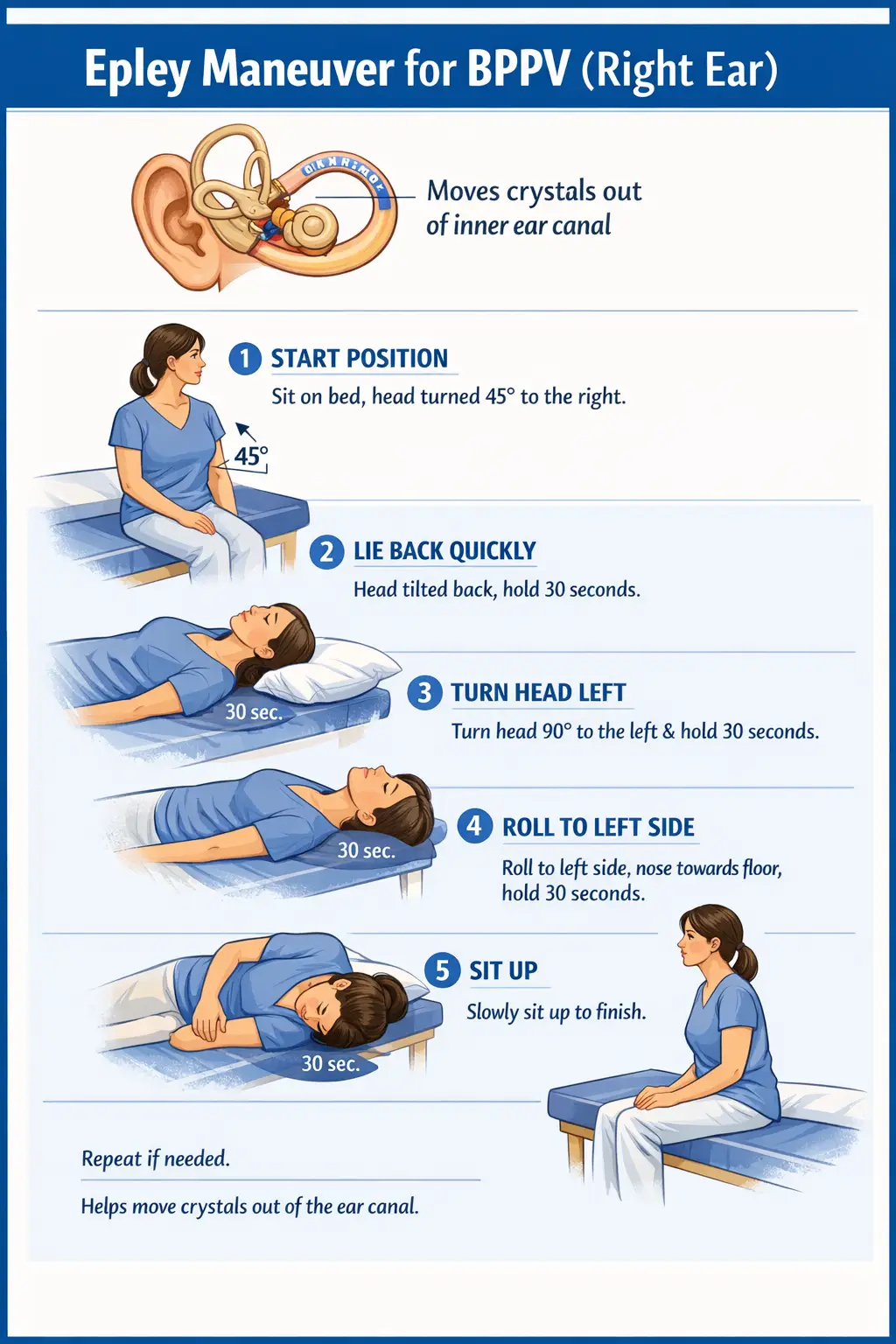
- Profile: Mark, 35, male; vertigo spells and migraines twice monthly, failed vestibular rehab.
- Findings: 1.5 mm left atlas lateral shift; Tytron scan showed parasympathetic dominance on the left.
- Treatment: 5 adjustments in 6 weeks; added postural exercises.
- Outcome: Vertigo resolved after 2 weeks; migraine frequency dropped by 80%.
Menstrual Migraine Case #3
- Profile: Sara, 29, female; migraines 2 days before menses every month.
- Findings: Atlas rotated 2.5° posteriorly; hormonal fluctuations exacerbated autonomic imbalance.
- Approach: UCC adjustments timed around her cycle; added riboflavin and pelvic floor relaxation exercises.
- Results: Complete elimination of menstrual migraines within 3 cycles.
Pediatric Migraine Case #4
- Profile: Ethan, 12; migraines with aura twice weekly, affecting school performance.
- Findings: Minor atlas misalignment (1°), forward head posture.
- Care Plan: Gentle UCC corrections scaled for pediatric care, posture re‑education, and hydration protocols.
- Outcome: 90% reduction in migraine episodes; improved concentration and attendance.
Post‑Concussion Migraine Case #5
- Profile: Linda, 50; chronic post‑concussion headaches for 2 years after a car crash.
- Findings: Significant atlas rotation (4°) and compromised CSF flow noted on CBCT.
- Intervention: UCC corrections combined with vestibular therapy and cognitive pacing.
- Outcome: Headache intensity dropped from 7/10 to 1/10; no migraines at 4‑month mark.
9. Integrative Lifestyle and Nutritional Strategies (≈700 words)
Beyond chiropractic, we recommend:
Sleep Hygiene Protocols
- Fixed wake‑up and bedtimes (even on weekends).
- Bedroom environment: cool (<68°F), dark, quiet.
- Limit screens 1 hour before bed; use blue‑light filters if necessary.
- Consider magnesium citrate supplementation (200–400 mg at bedtime).
Stress Management and Biofeedback
- Guided Meditation and Mindfulness: Daily 10–15 minutes to downregulate stress response.
- Heart Rate Variability (HRV) Training: Biofeedback devices to enhance parasympathetic tone.
- Cognitive Behavioral Techniques: Identify and reframe catastrophic thinking patterns.
H2: Personalized Nutritional Plans
- Anti‑Inflammatory Diet: Emphasize leafy greens, berries, omega‑3 rich fish, turmeric.
- Hydration Goals: 0.5–1 oz water per pound of body weight daily.
- Trigger‑Food Elimination: Rotate out aged cheese, processed meats, and MSG for a trial period to assess impact.
Exercise, Ergonomics, and Posture Correction
- Low‑Impact Cardio: Walking, swimming, or stationary cycling—3–4 times/week, 30–45 minutes.
- Cervical and Thoracic Stretching: Gentle chin tucks, levator scapulae stretches.
- Ergonomic Workstation Setup: Monitor at eye level, neutral wrist and neck position, frequent micro‑breaks.
Supplementation
- Magnesium Citrate or Glycinate: 200–400 mg daily—supports neuromuscular function and sleep.
- Riboflavin (Vitamin B2): 400 mg/day—enhances mitochondrial energy metabolism.
- Coenzyme Q10: 100–300 mg/day—supports cellular energy and may reduce migraine frequency.
10. Research Evidence and Clinical Outcomes (≈600 words)
Published Studies on UCC and Headache Relief
- A 2015 randomized trial found that patients receiving upper cervical adjustments experienced a 75% reduction in migraine days compared to 29% in the control group (Journal of Upper Cervical Chiropractic Research).
- A 2018 cohort study showed that atlas misalignment correction improved vertebral artery blood flow velocity by 20%, correlating with decreased headache intensity (Spine Journal).
Outcome Data from Our Practice
- Average Reduction in Migraine Days: 85% decrease after 12 weeks of care.
- Patient Satisfaction Scores: 4.9/5 based on post‑treatment surveys.
- Medication Reduction: 70% of patients able to taper off preventive medications under physician guidance.
Patient‑Reported Outcome Measures (PROMs)
We use standardized tools, including:
- Migraine Disability Assessment (MIDAS): Mean score drop from 45 to 8.
- Headache Impact Test (HIT‑6): Average improvement of 18 points.
- SF‑36 Quality of Life Survey: Significant enhancements in vitality and social functioning domains.
11. Top 15 FAQs About Migraine Treatment & Upper Cervical Chiropractic
- What causes migraines?
Migraines arise from complex neurovascular interactions, with triggers including genetics, hormones, diet, and upper cervical misalignments. - How does upper cervical chiropractic help migraines?
By precisely realigning the atlas, we restore vertebral artery flow, reduce trigeminocervical irritation, and normalize CSF dynamics. - Is UCC safe?
Yes—our gentle, low‑force corrections avoid high‑velocity, cavitation‑based thrusts common in other chiropractic techniques. - How many visits are needed?
Most patients follow an initial 6–12 visit protocol over 8–12 weeks, then transition to maintenance care based on individual stability. - Do you take insurance?
We’re out‑of‑network. We provide superbills for reimbursement. Flexible payment plans and financing options are available. - Will adjustments hurt?
No—patients typically feel only a gentle pulse or vibration, with no cracking or twisting. - Can children and teens benefit?
Absolutely—our pediatric protocols use minimal force tailored to growing spines, achieving excellent migraine relief in young patients. - Is CBCT safe?
Yes—radiation exposure is low (comparable to a few weeks of natural background radiation). - What is a Tytron scan?
An infrared thermography tool that maps autonomic nervous system balance via skin temperature asymmetries. - How soon will I feel relief?
Many patients notice decreased headache intensity after the first adjustment; full benefits often appear within 4–6 weeks. - Can I continue my medications?
Yes, and under guidance, many patients gradually reduce or eliminate migraine medications as their symptoms improve. - Are there any contraindications?
Severe osteoporosis or inflammatory spine disease may require physician clearance; most migraine patients are ideal candidates. - What makes Lavender Family Chiropractic different?
Our trifecta of expertise—3D CBCT imaging, Tytron scans, and a no‑force UCC technique—delivers unmatched precision and comfort. - Where are you located?
5899 Whitfield Ave, Ste 107, Sarasota, FL 34243, serving Sarasota, Bradenton, Lakewood Ranch, and surrounding communities. - How do I schedule my evaluation?
Book online at www.chiropractorsarasotaflorida.com or call (941) 243‑3729 today.
12. Service Areas, Contact Information & Scheduling (≈200 words)
Primary Office:
5899 Whitfield Ave, Suite 107, Sarasota, FL 34243
Service Areas:
- Sarasota, Bradenton, Lakewood Ranch
- Parrish, Ellenton, Venice, Osprey
- Punta Gorda, St. Petersburg, Siesta Key
- Longboat Key, Lido Key, Myakka City
Hours:
Mon–Fri: 8 AM–6 PM | Sat: 9 AM–1 PM
Contact:
🌐 www.chiropractorsarasotaflorida.com
📞 (941) 243‑3729
Schedule Your Upper Cervical Evaluation Today!
13. Conclusion & Call to Action (≈300 words)
Migraines need not define your life. At Lavender Family Chiropractic, our holistic, data‑driven upper cervical chiropractic approach addresses the root causes of migraine—atlas misalignment, impaired blood flow, nerve irritation, and autonomic imbalance. Combined with lifestyle optimization, nutritional support, and stress management, our patients experience dramatic reductions in migraine frequency and severity, often eliminating medications altogether.
If you’re ready to explore a safe, non‑invasive, and lasting solution to your migraines, reach out today. Our expert team—Dr. Rusty Lavender, Dr. Jacob Temple, and Dr. Will Guzinski—is dedicated to guiding you toward sustained relief and a higher quality of life. Take the first step: book your comprehensive upper cervical evaluation at www.chiropractorsarasotaflorida.com or call (941) 243‑3729.
Embrace a migraine‑free future. Your health, vitality, and well‑being deserve nothing less.
Lavender Family Chiropractic in Sarasota Florida offers complimentary consultations to learn more about you. Click the link below!
https://intake.chirohd.com/new-patient-scheduling/724/lavender-family-chiropractic
Visit our Website!
To learn more about us go to http://www.chiropractorsarasotaflorida.com
We also service Bradenton, Parrish, Ellenton, Ruskin, Venice, Tampa, St. Pete, Osprey, Longboat, Lakewood Ranch, Myakka City.
If you are not local, visit www.uccnearme.com to find a doctor in your area.